Patient Consent for Electronic Health Information Exchange
 Electronic health information exchange (eHIE) — the way that health care providers share and access health information using their computers — is changing rapidly. One way some providers share and access information is through a third-party organization called a health information exchange organization (HIE).
Electronic health information exchange (eHIE) — the way that health care providers share and access health information using their computers — is changing rapidly. One way some providers share and access information is through a third-party organization called a health information exchange organization (HIE).
HIEs help route information among various participating providers. In some HIEs, a provider can send out an electronic broadcast query that asks all provider participants whether they have information on a specific patient.
As eHIE increases, patient trust in HIEs must be ensured and patients may more often be asked to make a “consent decision.” This consent decision concerns the sharing and accessing of the patient’s health information through an HIE for treatment, payment, and health care operations purposes. When patients are asked to make consent decisions, we encourage providers, HIEs, and other health IT implementers to help patients make the consent decision meaningful.
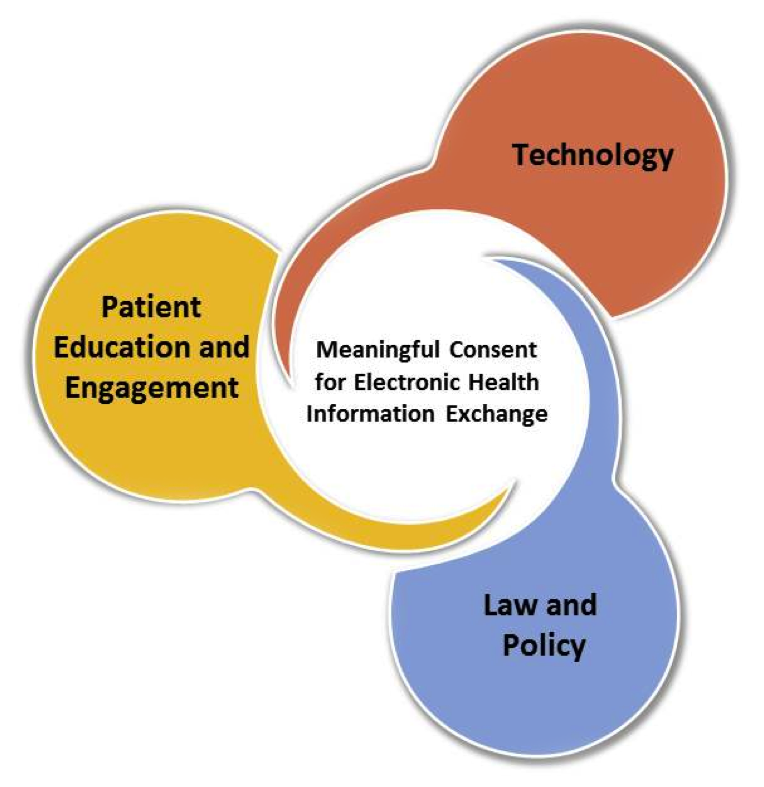
Implementers can enable meaningful consent by ensuring they consider the key parts displayed in the image to the right.
Patient Education and Engagement
Educating patients about topics including their consent options, who may release their information and how, and the significance of the consent choice.
Technology
Using technology to capture and maintain patient consent decisions, identify which sensitive portions of patient information are restricted from access, and communicate these restrictions electronically with others.
Law and Policy
Ensuring alignment with federal and state law and other legal and policy requirements pertaining to consent, personal choice, and confidentiality.
What is meaningful consent?
Consent should not be a “check-the-box” exercise. Meaningful consent occurs when the patient makes an informed decision and the choice is properly recorded and maintained. Specifically, the meaningful consent decision has six aspects. The decision should be:
- made with full transparency and education,
- made only after the patient has had sufficient time to review educational material,
- commensurate with circumstances for why health information is exchanged (i.e., the further the information-sharing strays from a reasonable patient expectation, the more time and education is required for the patient before he or she makes a decision),
- not used for discriminatory purposes or as a condition for receiving medical treatment,
- consistent with patient expectations, and
- revocable at any time.
Meaningful Consent Video Gallery
Visit our video gallery to learn more about the ONC eConsent Trial Project, which addressed patient questions surrounding consent and provided a way for patients to exercise their consent decisions electronically. View an overview of the project and sample patient experience, examples of patient education materials, and tutorials on using the eConsent Story Engine Tool.

Enabling Privacy: Data Segmentation
Data segmentation refers to the electronic labeling or tagging of a patient’s health information in a way that allows patients or providers to electronically share parts, but not all, of a patient record. Data segmentation plays a crucial role in enabling privacy of patient records.

eConsent Toolkit
The eConsent Trial Project, funded by ONC, developed and implemented electronic and innovative ways to:
- gather patients’ input on areas in which they want to learn more about consent,
- educate patients in a provider setting about the electronic sharing of their health information through an HIE, and
- capture and record choices patients make.

