Over the past several years, federal policy levers have been enacted to increase patient’s access to their health information. In 2014, hospitals were incentivized by the Centers for Medicare & Medicaid Services (CMS) Electronic Health Record (EHR) Incentive Program to adopt certified health IT that enabled patients to electronically view, download, and transmit their health information. In 2019, CMS required hospitals to provide their patients with the ability to access their health information via an application programming interface (API) using an app of their choice (1). In 2020, as part of the Cures Act Final Rule, the Office of the National Coordinator for Health Information Technology (ONC) established the Application Programming Interfaces (API) Condition and Maintenance of Certification, which seeks to minimize the “special effort” necessary to access, exchange, and use health electronic health information via certified API technology, (2). This data brief presents the 2021 national estimates on the proportion of U.S. hospitals that enabled patient electronic access to their health information.
HIGHLIGHTS
- Seven in ten hospitals enabled patients to access their health information using mobile or other software applications in 2021.
- Over half of hospitals enabled patient access through FHIR-based APIs in 2021.
- Over four in five hospitals enabled their patients to view their clinical notes in their patient portal in 2021.
- Small, Critical Access, rural, and independent hospitals enabled patient access to health information at lower rates compared to their counterparts.
- Nearly three quarters of hospitals using 2015 Edition Certified Health IT reported they provide patients access through apps using APIs.
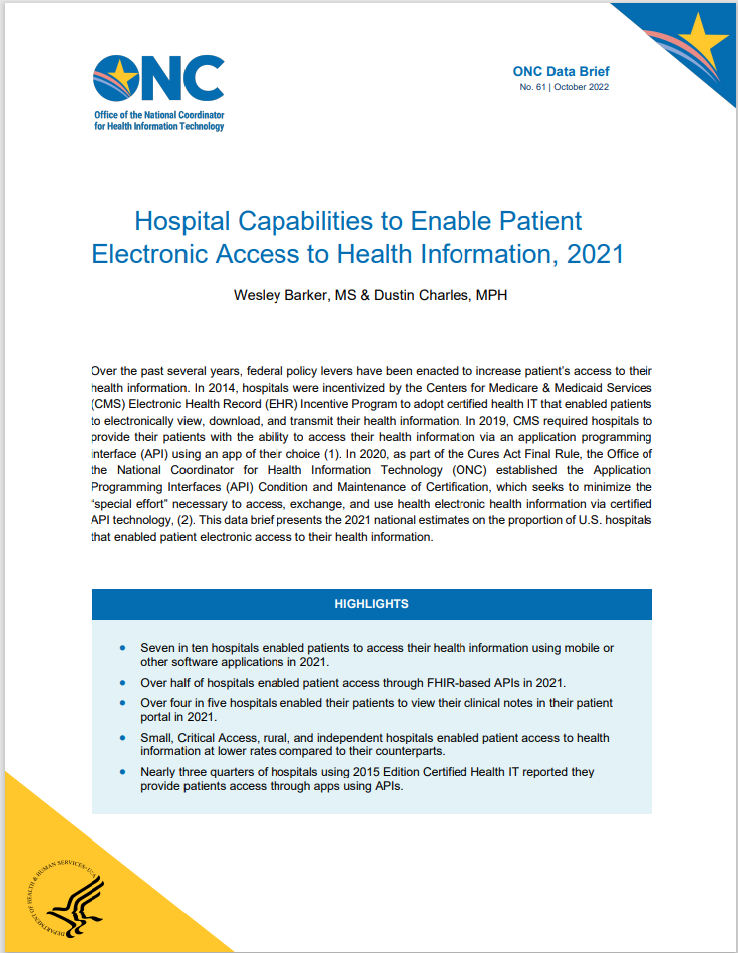
Seven in ten hospitals enabled patients to access their health information using an app in 2021.
FINDINGS
★ No change between 2019 and 2021 in the share of hospitals reporting that they enabled patients to access their health information using an app.
★ Small hospitals offered patients access through apps at a lower rate compared to medium-large hospitals in 2021.
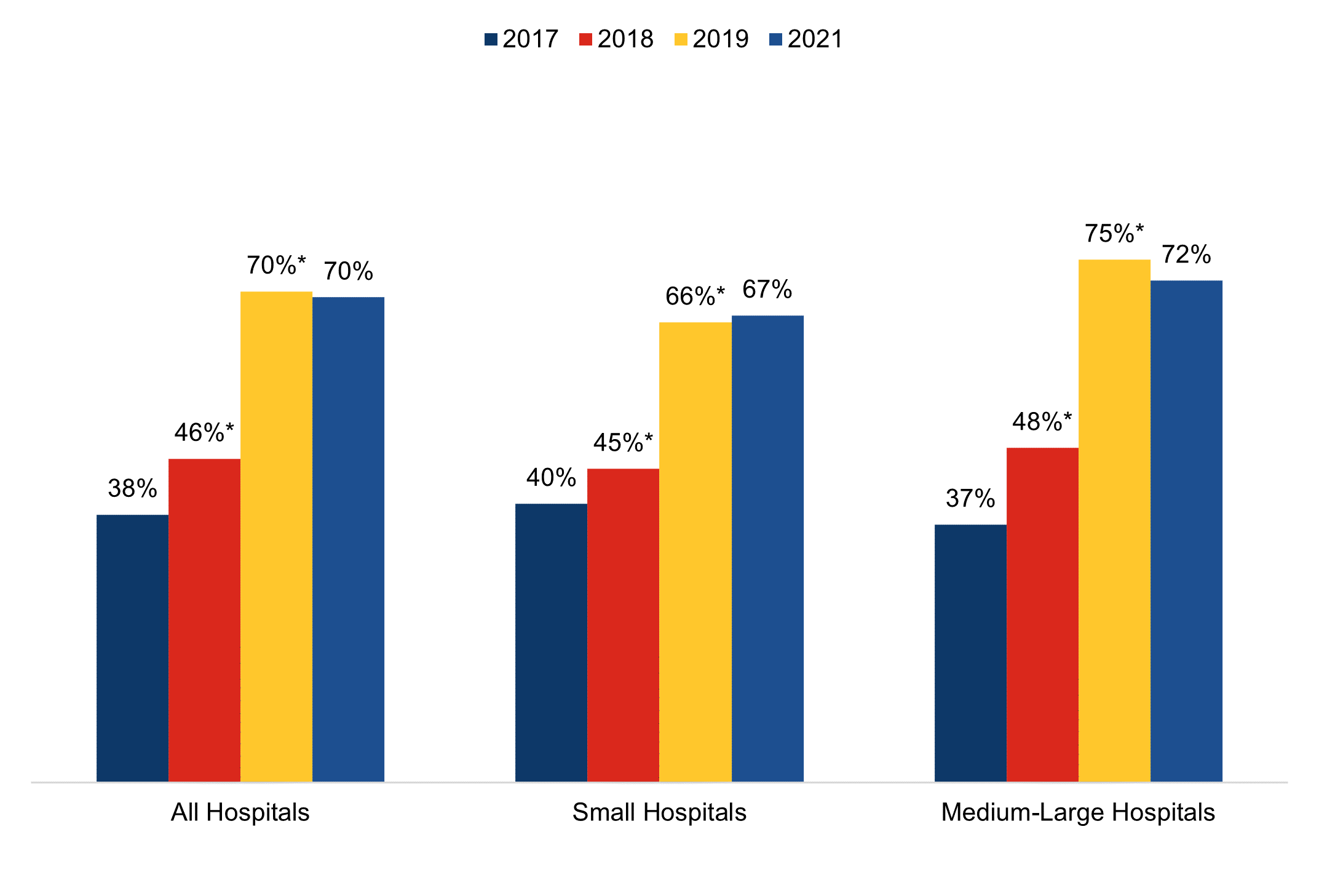
Figure 1: Percent of non-federal acute care hospitals that enabled patients who received inpatient care to access health information using applications configured to meet the application programming interface (API) specifications in the hospitals’ EHR, 2017-2021.
Source: AHA Annual Survey Information Technology Supplement.
Notes: Denominator represents all non-federal acute care hospitals that provide inpatient care. *Significantly different from previous year (p<0.05). The survey asked respondents about health information access for patients who received inpatient and outpatient care. Please refer to the Definitions section of this data brief for more information on the terminology. See Appendix Table A1 for survey questions related to inpatient and outpatient care.
Over half of hospitals enabled patient access through FHIR-based APIs in 2021.
FINDINGS
★ About 70% of hospitals reported that their patients can access their health information through an app.
★ Among hospitals that reported their patient can access their health information through an app, four in five supported FHIR API access for these apps.
Figure 2: Percent of non-federal acute care hospitals that enabled patients who received inpatient care to access health information using applications configured to meet the application programming interfaces (API) specifications in the hospitals’ EHR by API standard, 2021.
Source: AHA Annual Survey Information Technology Supplement.
Notes: Denominator represents all non-federal acute care hospitals that provide inpatient care. The survey asked respondents about health information access for patients who received inpatient and outpatient care. Please refer to the Definitions section of this data brief for more information on the terminology. See Appendix Table A1 for survey questions related to inpatient and outpatient care.
Small, Critical Access, rural, and independent hospitals enabled patients to access health information using apps at lower rates compared to their counterparts.
FINDINGS
★ Small, Critical Access, rural, and independent hospitals adopted certified technology that supports FHIR APIs at lower rates compared to their counterparts.
★ Nearly three quarters of hospitals using 2015 Edition Certified Health IT reported they provided patients access through apps using APIs.
★ Half of hospitals without technology from the “Top 3” EHR developers reported they did not provide app access to their patients.
| App Access Using a FHIR API | App Access Using a non-FHIR API | No App Access Using APIs | |
|---|---|---|---|
| Hospital Characteristics | |||
| Small (50%) | 49% | 18% | 33% |
| Medium-Large (50%) | 61%* | 11%* | 28%* |
| CAH(29%) | 46% | 20% | 34% |
| non-CAH (71%) | 59%* | 12%* | 29%* |
| Rural (40%) | 50% | 19% | 32% |
| Suburban-Urban (60%) | 58%* | 12%* | 30%* |
| Independent (33%) | 43% | 20% | 36% |
| System Affiliation (67%) | 61%* | 12%* | 27%* |
| Health IT Characteristics | |||
| No 2015 Edition (13%) | 37% | 10% | 53% |
| 2015 Edition (87%) | 57%* | 15%* | 28%* |
| Top 3 EHRs (79%) | 62%* | 13%* | 25%* |
| Next 3 EHRs (17%) | 36% | 22% | 42% |
| All other EHRs (4%) | 5% | 11% | 84% |
Table 1: Percent of non-federal acute care hospitals that enabled patients who received inpatient care to access health information through an app by hospital and health IT characteristics, 2021.
Source: AHA Annual Survey Information Technology Supplement.
Notes: Denominator represents all non-federal acute care hospitals that provide inpatient care. *Significantly different from corresponding category in the row below (p<0.05). The survey asked respondents about health information access for patients who received inpatient and outpatient care. The “Top 3” and “Next 3” EHRs were determined using data reported by hospitals in the 2021 survey. Please refer to the Definitions section of this data brief for more information on the terminology. See Appendix Table A1 for survey questions related to inpatient and outpatient care.
Over 4 in 5 hospitals enabled patients to view their clinical notes in their portal in 2021.
FINDINGS
★The percentage of hospitals who enabled patients to view their clinical notes increased by almost 50% from 2018 to 2021.
★ Small hospitals enabled patients to view their clinical notes at a lower rate compared to medium-large hospitals in 2021.
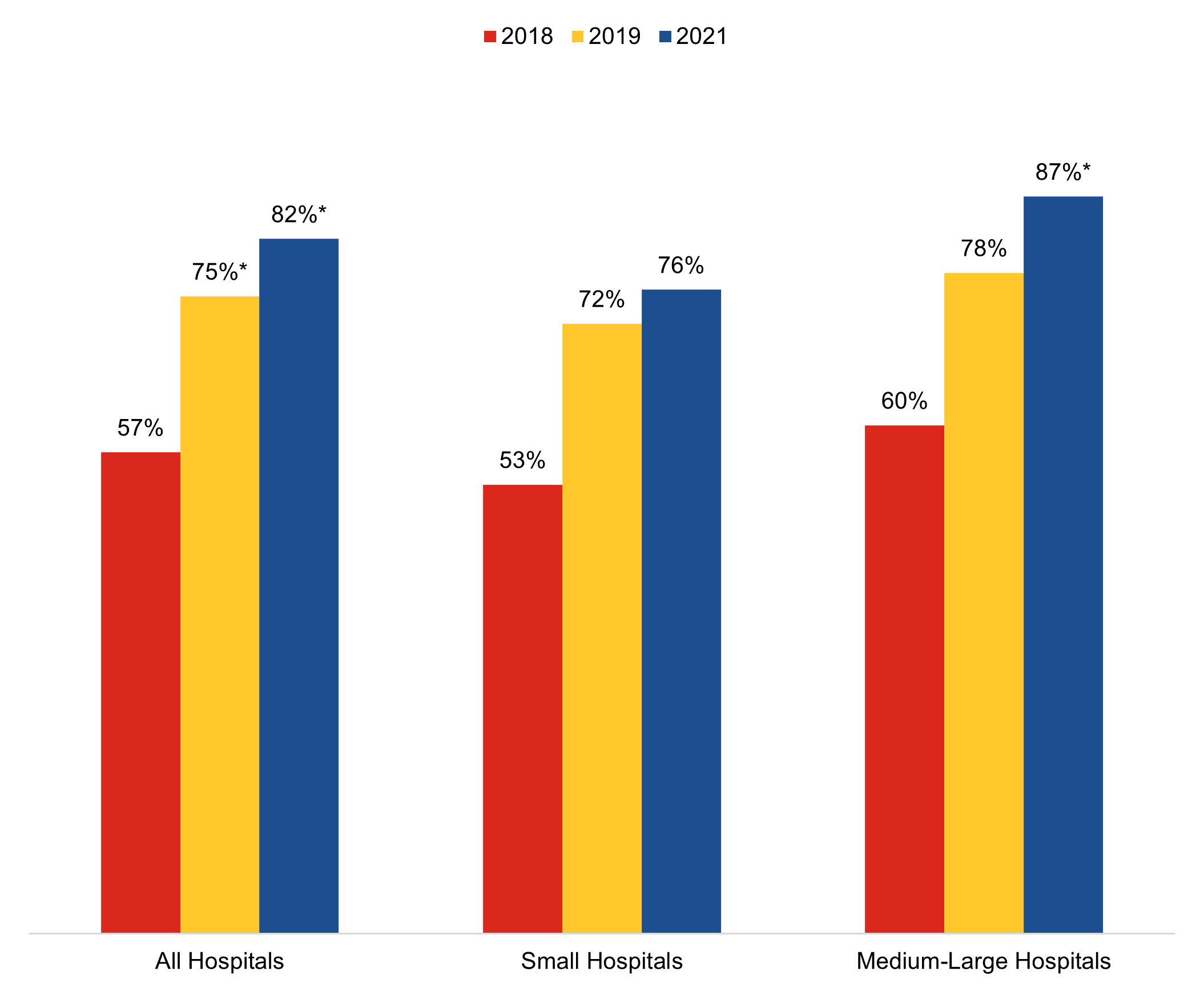
Figure 3: Percent of non-federal acute care hospitals that enabled patients who received inpatient care to view their clinical notes in their patient portal, 2021.
Source: AHA Annual Survey Information Technology Supplement.
Notes: Denominator represents all non-federal acute care hospitals that provide inpatient care. *Significantly different from previous year (p<0.05). The survey asked respondents about health information access for patients who received inpatient and outpatient care. Please refer to the Definitions section of this data brief for more information on the terminology. See Appendix Table A1 for survey questions related to inpatient and outpatient care.
Summary
Patient medical records are now digitized across nearly all hospitals in the U.S. (3). Federal programs, such as the CMS Promoting Interoperability Program (formerly known as the Medicare and Medicaid EHR Incentive Program), have helped incent hospitals to adopt certified health IT that enables patients to access their health information electronically. The 21st Century Cures Act further builds on this foundation and modernizes the methods patients can use to access their health information and the ways their health care providers can enable this electronic access (4). ONC’s Health IT Certification Program 2015 Edition certified application programming interface (API) technology enables patients to access their health information using smartphone and web applications. In 2021, 9 in 10 hospitals possessed 2015 Edition certified EHR technology, and 7 in 10 hospitals reported they provided patients access to their health information through the app of their choice via the certified API technology, the same rate we found in 2019 (5). These are high rates of adoption, but we found significant disparities in the implementation of this functionality across hospitals.
Consistent with past findings, small, Critical Access, rural, and independent hospitals enabled patient electronic access to health information using both portals and APIs at lower rates than other hospitals (5). Patients served by small, Critical Access, rural, and independent hospitals are less likely to have access to their health information through an app of their choice. Furthermore, half of hospitals without technology from the “Top 3” EHR developers reported they did not provide app access to their patients. This indicates that there are gaps in access due to hospital resources, technical knowledge, and other technology issues unrelated to the capabilities of certified EHRs. Some hospitals may have the API technology enabled, but few or no app developers have connected to their EHR. Market effects, particularly app developers targeting the clients of the EHR market leaders, who have adopted standards-based APIs, may be at play. We expect that some of these challenges may be ameliorated as new certification requirements come into effect and developers of certified health IT upgrade and provide standards-based APIs to their customers no later than December 31, 2022 (6).
In particular, certified API technology developers must rollout APIs that support Release 4 of the Fast Healthcare Interoperability Resources (FHIR) standard by the end of 2022. We’ve found that market leaders largely supported the standard for their 2015 Edition certified API technology (7), but the data show that, among hospitals with one of the three market leading EHRs, 1 in 4 did not provide their patients app access. Research shows that standards-based APIs and improved access to the APIs’ technical requirements, documentation, and testing processes can lower barriers to entry for app developers and create a more level playing field (8). These requirements, including the new United States Core Data for Interoperability (USCDI) v1 standard, are intended to create more predictability and uniformity for app developers. The availability of standards-based APIs across all certified API technology will make it easier for app developers to build their technology around these standards and integrate across all these certified technologies. New requirements should, also, invite more competition.
As certified developers are required to meet new certification requirements - transitioning to a uniform data standard and minimum set of documentation requirements - there may be a positive effect on the availability of apps and their ability to connect to the hospitals’ EHR APIs, leading to an increase in app access and connectivity. CMS also requires all CMS-regulated payers to implement and maintain a secure, standards-based API that allows patients to easily access their claims and encounter information through third-party applications of their choice (9). This further expands patients’ ability to gather and use their health care information using modern, internet-based tools. Finally, as clinical notes are a required data class in the USCDI, we expect patient access to these notes to continue to increase as they become a standard part of the data patients can access through the app of their choice and through their health care provider’s patient portal. As these requirements take effect, it will be important to continue to monitor these trends to ensure hospitals enable patients with technology and health information access to better manage their health care.
DEFINITIONS
Non-federal acute care hospital: Hospitals that meet the following criteria: acute care general medical and surgical, children’s general, and cancer hospitals owned by private/not-for-profit, investor-owned/for-profit, or state/local government and located within the 50 states and District of Columbia.
Small hospital: Non-federal acute care hospitals of bed sizes of 100 or less.
Rural hospital: Hospitals located in a non-metropolitan statistical area.
Critical Access Hospital: Hospitals with less than 25 beds and at least 35 miles away from another general or critical access hospital.
System affiliated hospital: A system is defined as either a multi-hospital or a diversified single hospital system. A multi-hospital system is two or more hospitals owned, leased, sponsored, or contract managed by a central organization. Single, freestanding hospitals may be categorized as a system by bringing into membership three or more, and at least 25 percent, of their owned or leased non-hospital pre-acute or post-acute health care organizations.
Inpatient: A patient who is admitted to a hospital to undergo treatment. The survey asks about “patients who receive inpatient care provided by your hospital”. Inpatients refer to patients who receive inpatient care from respondent hospital. Please refer to Appendix Table A1 to review the applicable questions.
Outpatient: A patient who receives treatment and is not admitted to a hospital. The survey asks about “patients who receive outpatient care provided by your hospital”. Outpatients refer to patients who receive outpatient care from respondent hospital. Please refer to Appendix Table A1 to review the applicable questions.
Outpatient sites: Sites or locations within a hospital’s campus or care facility that provide outpatient treatment. These sites may include emergency rooms, laboratories, and imaging rooms.
2015 Edition Certified Electronic Health Record (EHR): An EHR that meets certification criteria requirements established by the U.S. Department of Health and Human Services. These criteria establish the required capabilities, standards, and implementation specifications that health information technology needs to meet in order to become certified under the ONC Health IT Certification Program. Certified health IT products can be used for participation in CMS quality reporting programs and State Promoting Interoperability Programs.
Top 3 EHRs: The “Top 3” represent the three health IT developers with the most hospital clients. These developers are Cerner Corporation, Epic Systems Corporation, and MEDITECH. The market share is based off hospital responses to the 2021 survey.
Next 3 EHRs: The “Next 3” represent the three health IT developers with the second most hospital clients. These developers are Allscripts, CPSI, and MEDHOST. The market share is based off hospital responses to the 2021 survey.
Data Source and Methods
Data are from the American Hospital Association (AHA) Information Technology (IT) Supplement to the AHA Annual Survey. Since 2008, ONC has partnered with the AHA to measure the adoption and use of health IT in U.S. hospitals. ONC funded the 2021 AHA IT Supplement to track hospital adoption and use of EHRs and the exchange of clinical data.
The chief executive officer of each U.S. hospital was invited to participate in the survey regardless of AHA membership status. The person most knowledgeable about the hospital’s health IT (typically the chief information officer) was requested to provide the information via a mail survey or secure online site. Non-respondents received follow-up mailings and phone calls to encourage response.
This brief reports results from the 2017, 2018, 2019, and 2020 AHA IT Supplement. The 2017 survey was fielded from January 2018 to May 2018; the 2018 survey was fielded from January 2019 to May 2019; and the 2019 survey was fielded from January 2020 to June 2020. Due to pandemic-related delays, the 2020 survey was not fielded on time and was fielded from April 2021 to September 2021. Since the IT supplement survey instructed respondents to answer questions as of the day the survey is completed, we refer to responses to the 2020 IT supplement survey as happening in 2021 in this brief. The response rate for non-federal acute care hospitals for the 2020 survey was 54 percent. A logistic regression model was used to predict the propensity of survey response as a function of hospital characteristics, including size, ownership, teaching status, system membership, and availability of a cardiac intensive care unit, urban status, and region. Hospital-level weights were derived by the inverse of the predicted propensity.
References
- Centers for Medicare and Medicaid Services (CMS). Promoting Interoperability Programs. https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms.
- Office of the National Coordinator for Health Information Technology. Certification Companion Guide: Application Programming Interfaces. https://www.healthit.gov/condition-ccg/application-programming-interfaces.
- Office of the National Coordinator for Health Information Technology. ‘National Trends in Hospital and Physician Adoption of Electronic Health Records,’ Health IT Quick-Stat #61. March 2022. https://www.healthit.gov/data/quickstats/national-trends-hospital-and-physician-adoption-electronic-health-records.
- 21st Century Cures Act, section 4006. https://www.gpo.gov/fdsys/pkg/PLAW-114publ255/pdf/PLAW-114publ255.pdf.
- Johnson C. & Barker W. (June 2021). Hospital Capabilities to Enable Patient Electronic Access to Health Information, 2019. ONC Data Brief, no.55. Office of the National Coordinator for Health Information Technology: Washington DC.
- Office of the National Coordinator for Health IT. ONC Cures Act Final Rule. https://www.federalregister.gov/documents/2020/05/01/2020-07419/21st-century-cures-act-interoperability-information-blocking-and-the-onc-health-it-certification.
- Posnack S. & Barker W. ‘The Heat is On: US Caught FHIR in 2019.’ ONC Buzz Blog. https://www.healthit.gov/buzz-blog/health-it/the-heat-is-on-us-caught-fhir-in-2019.
- Office of the National Coordinator for Health Information Technology. ‘Accelerating Application Programming Interfaces for Scientific Discovery: App Developer and Data Integrator Perspectives.’ March 2022. https://www.healthit.gov/sites/default/files/page/2022-06/App-Developer-and-Integrator-Perspectives.pdf.
- Centers for Medicare and Medicaid Services (CMS). Interoperability and Patient Access Fact Sheet. https://www.cms.gov/newsroom/fact-sheets/interoperability-and-patient-access-fact-sheet.
Acknowledgements
The authors are with the Office of Technology, within the Office of the National Coordinator for Health Information Technology.
Suggested Citation
Barker W. & Charles D. (October 2022). Hospital Capabilities to Enable Patient Electronic Access to Health Information, 2021. ONC Data Brief, no.61. Office of the National Coordinator for Health Information Technology: Washington DC.
Appendix
Appendix Table A1: Survey questions assessing hospital capabilities to enable patient electronic access to health information
| Question Text | Response Options |
|---|---|
| Are patients who receive care provided by your hospital or outpatient sites able to do the following: (Check “Yes” only if the functionality has been “turned on” and is fully implemented and available to patients.) | Yes | No | Do not know • View their health/medical information online in your portal • Download health/medical information from their medical record from your portal • Import their medical records from other organizations into your portal • Electronically transmit (send) health/medical information to a third party from your portal • View their inpatient clinical notes (e.g. discharge summary) in their portal • Access their health/medical information using applications (apps) configured to meet the application programming interfaces (API) specifications in your EHR • Access their health/medical information using applications (apps) configured to meet Fast Healthcare Interoperability Resource (FHIR) specifications |
Appendix Table A2: Percent of non-federal acute care hospitals that enabled patients to view, download, and transmit health information in their portal, 2012-2021.
| Year | View | Download | Transmit | VD&T |
|---|---|---|---|---|
| 2012 | 24% | 14% | - | - |
| 2013 | 40%* | 28%* | 12% | 10% |
| 2014 | 91%* | 82%* | 66%* | 64%* |
| 2015 | 95%* | 87%* | 71%* | 69%* |
| 2016 | 96% | 87% | 74%* | 71%* |
| 2017 | 97% | 91%* | 74% | 72% |
| 2018 | 97% | 91% | 73% | 71% |
| 2019 | 97% | 91% | 75%* | 73%* |
| 2021 | 96% | 92% | 76% | 74% |
Source: AHA Annual Survey Information Technology Supplement.
Note: *Statistically significantly different from prior year (p < 0.05).
Appendix Table A3: Percent of non-federal acute care hospitals that enabled patients to view, download, and transmit health information in their portal by hospital characteristics, 2021.
| Hospital Characteristics | View | Download | Transmit | VD&T |
|---|---|---|---|---|
| Overall | 96% | 92% | 76% | 74% |
| Small (50%) | 93% | 88% | 70% | 67% |
| Medium-Large (50%) | 98%* | 96%* | 83%* | 81%* |
| CAH (29%) | 92% | 87% | 65% | 62% |
| non-CAH (71%) | 97%* | 94%* | 81%* | 79%* |
| Rural (40%) | 93% | 89% | 69% | 66% |
| Suburban-Urban (60%) | 97%* | 94%* | 81%* | 79%* |
| Independent (33%) | 91% | 85% | 65% | 61% |
| System Affiliation (67%) | 98%* | 95%* | 82%* | 80%* |
| Top 3 EHR (79%) | 98%^ | 96%^ | 82%^ | 80%^ |
| Next 3 EHR (17%) | 91% | 82% | 61% | 56% |
| All other EHRs (4%) | 69% | 52% | 34% | 28% |
Source: AHA Annual Survey Information Technology Supplement.
Note: *Statistically significantly different from prior year (p < 0.05).