Family medicine physicians can play an important role in addressing social factors that impact health and health equity (1). Family physicians often provide care for individuals in medically underserved communities (2) and are well-positioned to collect information on patients’ health-related social needs and social determinants of health (SDOH) that can be used to inform clinical-decision making, refer patients to social services, and identify health inequities. Collectively, these health equity data can help care teams identify and address health disparities and improve patient and population health (3). This brief uses data from 3 years (2022-2024) of the American Board of Family Medicine’s Continuous Certification Questionnaire, which is fielded as two separate modules to mitigate participant burden. Using data from one module, we describe methods physicians use to document social needs in their electronic health record (EHR) system, particularly structured methods that facilitate data sharing with other organizations. Using data from a second module, we describe family physicians’ rated importance of having access to external SDOH data from other organizations and how this varies by patient population and availability of resources to address social needs. Together, findings provide insight into the ability of family medicine practices to address social factors that impact health and health equity.
HIGHLIGHTS
- In 2022-2024, most family physicians who documented social needs in their electronic health record (EHR) system used a combination of free-text notes and structured methods, such as checking a box/button or entering it as a diagnosis.
- Physicians in small, independently owned practices had lower rates of social needs documentation in the EHR—especially using structured methods—compared to those in large, academic health centers or hospitals.
- Nearly all family physicians nationally rated their access to external social determinants of health (SDOH) data to be very or somewhat important, especially those serving vulnerable patient populations as these physicians may have greater awareness of how SDOH can impact their patients’ health and care.
- Physicians who reported their clinic has resources available to address social needs had higher rates of structured documentation and placed greater importance on having access to external SDOH data, indicating a relationship between how data are captured and received and whether those data can be used to improve patient and population health.
In 2024, over half of family physicians used structured methods—check boxes/buttons or diagnosis codes—to document social needs in the EHR.
FINDINGS
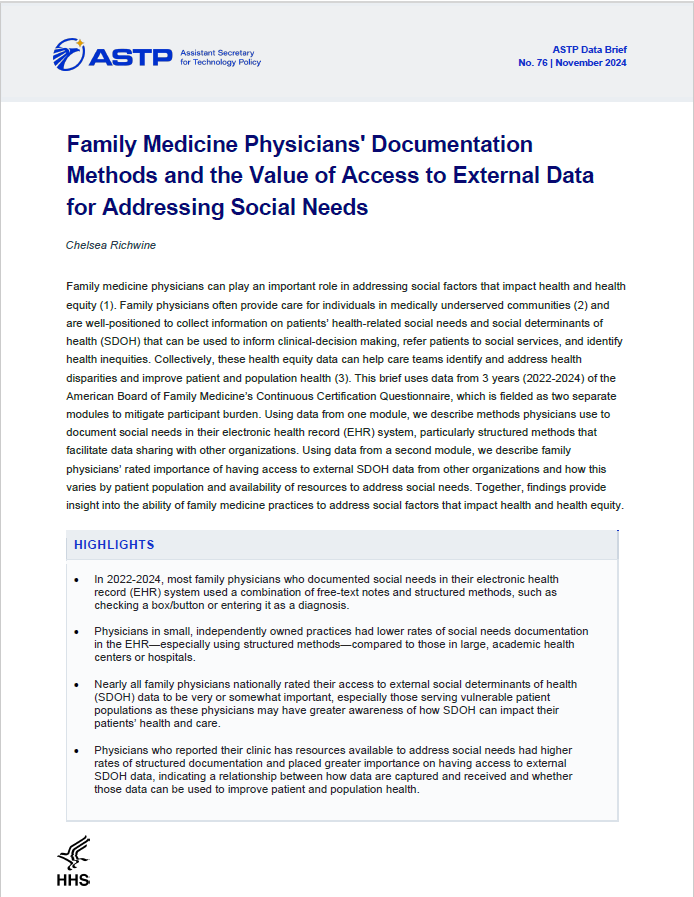
★ In 2024, 60% of family physicians used free-text notes to document social needs in their EHR, a slight decrease from 2022 and 2023.
★ Documenting social needs by checking a box/button in the EHR was more common than entering it as a diagnosis (i.e., ICD-10-CM Z codes). However, both types of structured documentation methods increased significantly between 2023 and 2024.
★ Overall, family physicians’ use of structured methods—checkboxes/buttons or diagnosis codes— to document social needs is on the rise, with 58% using at least one structured method in 2024, a significant increase from 55% in 2023.
Figure 1: Trends in the methods family physicians often or sometimes use to document screening for social needs in primary outpatient EHR, 2022-2024.
Source: 2022-2024 American Board of Family Medicine Continuous Certification Questionnaire
Notes: The denominator represents family physicians who use an EHR. This includes Module B respondents in 2022 (N = 2,066) and 2023 (N = 4,109), and all respondents in 2024 (N = 7,620). “Structured methods” = an aggregate measure indicating respondents who often or sometimes used checkbox/button or diagnosis codes to document social needs in the EHR. *Indicates statistically significant difference from prior year (P<.05). ). See Appendix Table 1 for survey questions and Data Sources and Methods for respondent population.
Most family physicians who document social needs in their EHR use a combination of free-text notes and structured documentation methods.
FINDINGS
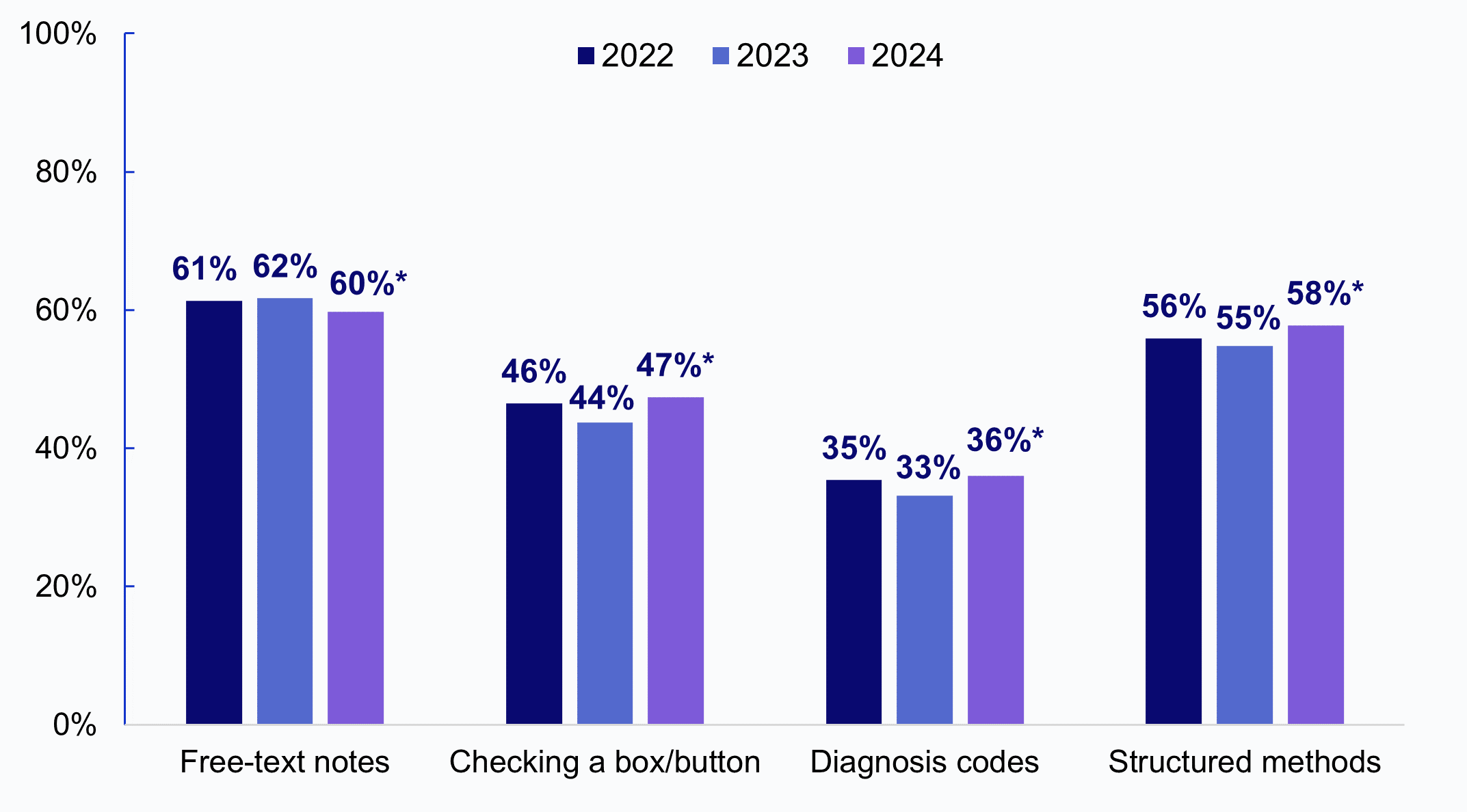
★ While free-text notes remain the most common method used by family physicians to document social needs in the EHR, only 16% of physicians used this method exclusively.
★ Nearly half of family physicians (44%) used free-text notes in combination with at least one structured method—checkbox/button (13%), diagnosis codes (9%) or both (22%)—to document social needs in their EHR. Only 13% used structured methods exclusively.
★ About a quarter of family physicians (27%) did not document social needs in their EHR.
Figure 2: Combination of methods family physicians often or sometimes use to document screening for social needs in primary outpatient EHR, 2022-2024 (pooled).
Source: 2022-2024 American Board of Family Medicine Continuous Certification Questionnaire
Notes: The denominator represents a pooled sample of family physicians from 2022-2024 who use an EHR (N = 13,795). This includes Module B respondents in 2022-2023 (N = 6,175) and all respondents in 2024 (N = 7,620). See Appendix Table 1 for survey questions and Data Sources and Methods for respondent population. See Appendix Table 2 for a simplified exposition of these relationships.
Physicians in small, independent practices had lower rates of EHR documentation using any method compared to those in large, academic health centers or hospitals.
FINDINGS
★ Family physicians in academic health centers and those serving a large share (>50%) of vulnerable patients had the highest rates of any social needs documentation in the EHR (83% and 82%, respectively) and using structured methods (67% and 66%, respectively).
★ Family physicians in independent practices, serving a small share (<10%) of vulnerable patients, and those not participating in value-based care had the lowest rates of any (67%, 66%, and 61%, respectively) and structured documentation (48%, 50%, and 39%, respectively).
★ Family physicians using one of the top 3 EHR vendors by market share had higher rates of any (75%) and structured documentation (60%) compared to those using smaller vendors.
Table 1: Methods family physicians often or sometimes use to document screening for social needs in primary outpatient EHR, by practice characteristics, 2022-2024 (pooled).
Any documentation in EHR (73%) | Structured documentation (57%) | |
|---|---|---|
Practice site | ||
Academic health center (ref) | 83% | 67% |
Government | 80% | 67% |
Hospital/health system | 74%* | 59%* |
Independent | 67%* | 48%* |
Other | 69%* | 53%* |
Practice size | ||
1 to 5 (ref) | 70% | 53% |
6 to 10 | 76%* | 61%* |
>20 | 73%* | 58%* |
Location | ||
Rural | 73% | 54% |
Urban | 73% | 57%* |
Value-based care | ||
Yes (ref) | 77% | 62% |
No | 61%* | 39%* |
Don't know | 64%* | 47%* |
Vulnerable patient pop % | ||
<10% (ref) | 66% | 50% |
10-49% | 74%* | 57%* |
>50% | 82%* | 66%* |
EHR vendor market share^ | ||
Top 3 vendors by market share (ref) | 75% | 60% |
4th to 6th market position | 72%* | 54%* |
7th to 9th market position | 68%* | 49%* |
All other vendors | 69%* | 49%* |
Source: 2022-2024 American Board of Family Medicine Continuous Certification Questionnaire
Notes: “Any documentation in EHR” = often or sometimes used at least 1 of 3 methods in Figure 1 to document social needs in the EHR. Structured documentation = often or sometimes used structured methods (checkbox/button or diagnosis codes) to document social needs in the EHR. *Indicates statistically significant difference from reference category (P<.05). See Appendix Table 1 for survey questions and Data Sources and Methods for respondent population. ^ EHR vendor market share is based on a question in the survey asking respondents to indicate their outpatient EHR vendor.
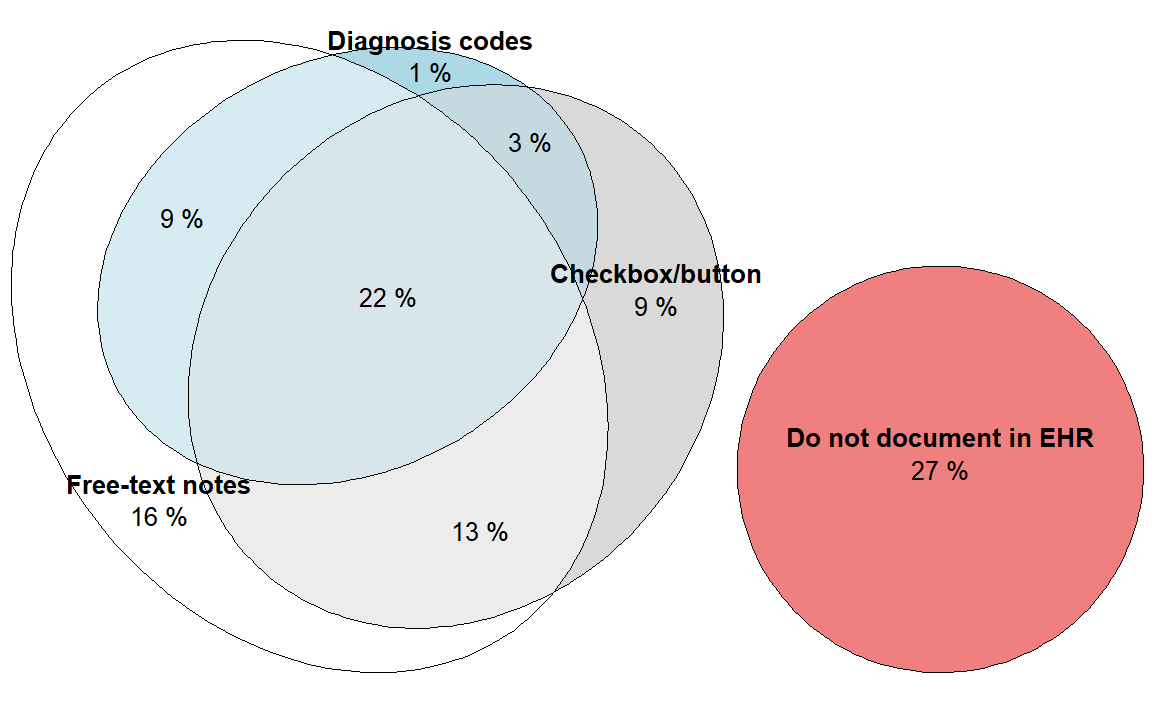
In 2022 and 2023, nearly all family physicians nationally rated their access to external SDOH data to be very or somewhat important.
FINDINGS
★ While less than half of family physicians rated their access to external SDOH data to be “very important” – the vast majority of physicians felt it was at least somewhat important to have access to external SDOH data (e.g., housing stability, food insecurity) from other health systems/organizations.
★ While less than 1 in 10 family physicians rated their access to external SDOH data to be “not at all important,” this may be reflective of the patient populations they serve (e.g., low prevalence of social needs) or greater reliance on data collected internally.
Figure 3: Family physicians’ rated importance of having access to external SDOH data from other health systems/organizations, 2022-2023.
Source: 2022-2023 American Board of Family Medicine Continuous Certification Questionnaire
Notes: Denominator represents family physicians who responded to Module A of each survey and use an EHR (N = 2,088 in 2022 and N = 4,087 in 2023). Question was not asked in 2024. *Indicates statistically significant difference from prior year (P<.05). See Appendix Table 1 for survey questions and Data Sources and Methods for respondent population.
Physicians serving a higher share of vulnerable patients placed greater importance on having access to external SDOH data.
FINDINGS
★ In 2022-2023, family physicians serving a large (>50%) or moderate (10-49%) share of vulnerable patients had higher rates of indicating it is “very important” to have access to external SDOH data (47% and 42%, respectively) compared to those with a small share (<10%) of vulnerable patients (38%).
★ Sixty-two percent of family physicians with a small share of vulnerable patients (<10%) indicated it was somewhat (53%) or not at all important (9%) to have access to external SDOH.
Figure 4: Family physicians’ rated importance of having access to external SDOH data from other health systems/organizations, by share of vulnerable patient population, 2022-2023 (pooled).
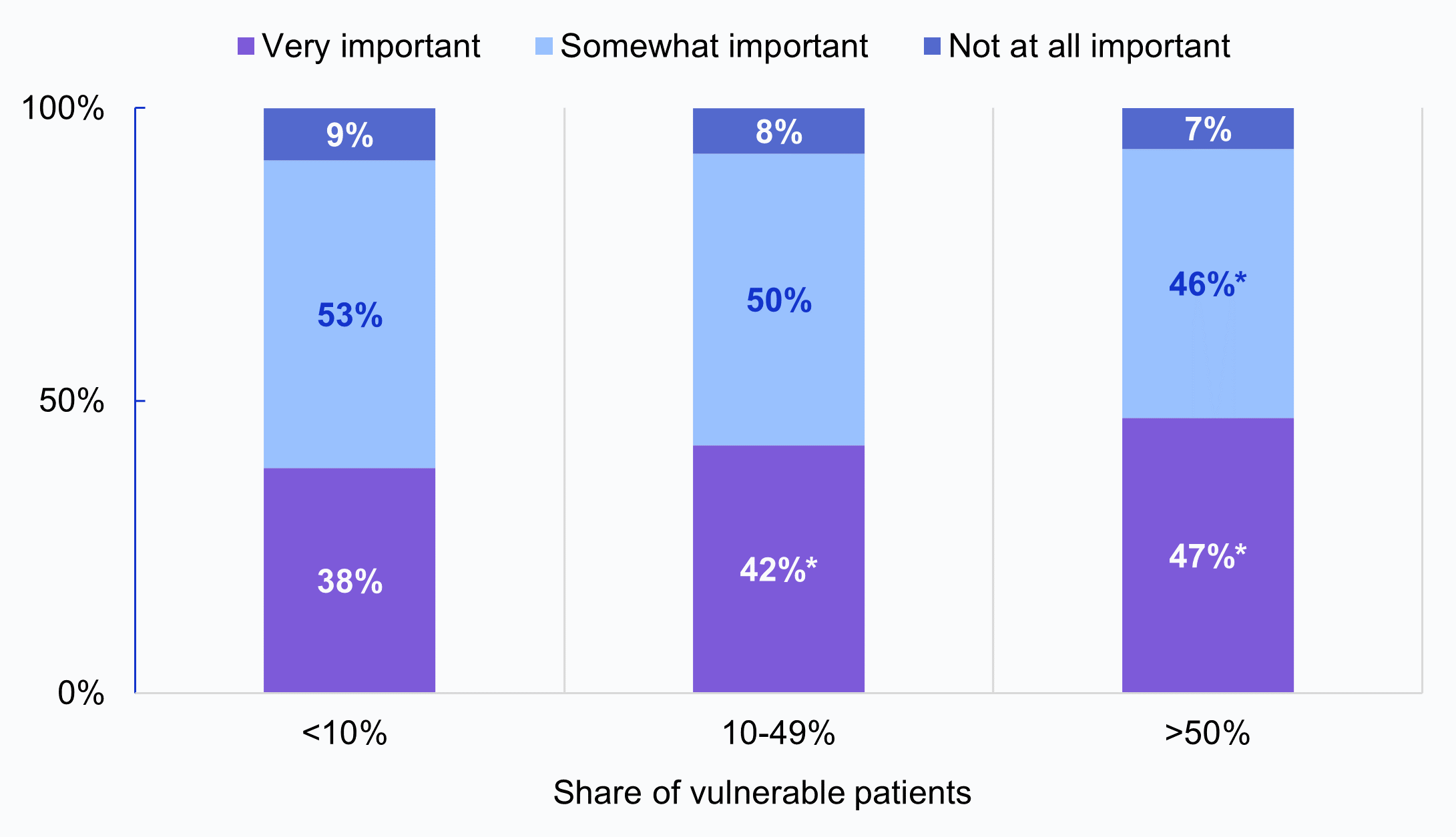
Source: 2022-2023 American Board of Family Medicine Continuous Certification Questionnaire
Notes: The denominator represents a pooled sample of family physicians from 2022-2023 who use an EHR (N = 6,175), grouped by <10% vulnerable patients (N = 2,160, 35%), 10-49% vulnerable patients (N = 2,662, 43%), and >50% vulnerable patients (N = 1,353, 22%). *Indicates statistically significant difference from reference group (<10% vulnerable patients) (P<.05). See Appendix Table 1 for survey questions and Data Sources and Methods for respondent population.
Family physicians who reported their clinic had resources to address social needs placed greater importance on having access to external SDOH data and had higher rates of structured documentation.
FINDINGS
★ Family physicians who reported their clinic had resources—such as dedicated staff and linkages to community programs—to address social needs (Appendix Figure 1) had higher rates of indicating it is “very important” to have access to external SDOH data (44%) compared to those who do not have resources available (40%) (Panel A).
★ Family physicians who reported their clinic had resources to address social needs also had higher rates of using structured methods to document social needs (65%)—which may facilitate data sharing with other providers or community-based organizations—compared to those who do not have resources available (41%) (Panel B).
Figure 5: Family physicians’ rated importance of having access to external SDOH data (Panel A) and use of structured methods to document social needs (Panel B), by availability of resources and tools to address patients' social needs.
Panel A: Importance of Access to External SDOH Panel B: Use of structured methods to document social needs
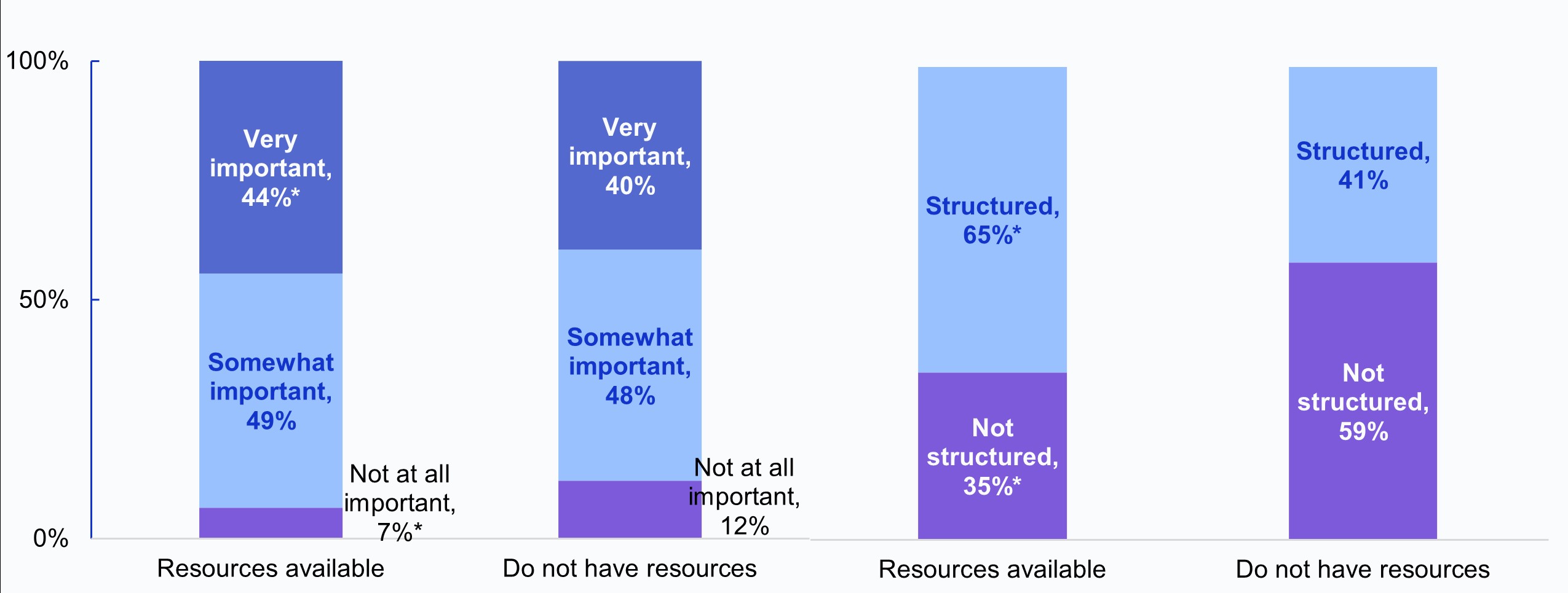
Source: 2022-2023 (Panel A) and 2022-2024 (Panel B) American Board of Family Medicine Continuous Certification Questionnaire
Notes: The denominators in Panels A and B represent a pooled sample of family physicians who use an EHR from 2022-2023 (N = 6,175) and 2022-2024 (N = 13,795), respectively, grouped by those who indicated they agree their clinic has “Resources available” to address social needs (56% of the full sample) and those who disagree and “Do not have resources” to address social needs (23% of the full sample). Neutral responses (neither agree nor disagree) are not reported (22% of the full sample). *Indicates statistically significant difference between groups (P<.05). See Appendix Table 1 for survey questions and Data Sources and Methods for respondent population.
SUMMARY
Family physicians can play an important role in addressing the social risk factors that impact the health of patients and communities by screening for individuals’ health-related social needs and broader SDOH. Data captured through screening can be used to inform clinical decision-making, refer patients to social services or resources, and identify and address health inequities in the community. In 2022-2024, nearly three-quarters of physicians (73%) used at least one of three methods—free-text notes, checkbox/button, diagnosis codes—to document social needs in their EHR. While more than half of family physicians (61%) used free-text notes to document social needs in the EHR, only 16% used this method exclusively, and 44% used free-text notes in combination with at least one structured method. Our findings suggest the use of structured methods are on the rise with 58% of family physicians using at least one of two structured documentation methods in 2024, yet it is unclear how often these methods are used or which data elements are more commonly captured using structured electronic screening tools vs. free-text documentation. It is also unclear whether or how the introduction of new screening requirements and financial incentives to conduct SDOH screening assessments shape methods of documentation and perceived value of having access to data from outside sources.
While over half of physicians used structured methods to document social needs screening in their EHR, documentation practices varied by physician practice characteristics, patient population, and perceived capacity to address social needs. This is consistent with findings from a recent study of office-based physicians that demonstrated variation in documentation practices by physician specialty and practice characteristics (4). Our findings indicate that between 2022-2024, family physicians in small, independently-owned practices had lower rates of EHR documentation overall and using structured methods compared to those in large, academic health centers or hospitals, which may reflect differences in availability of resources to identify or address social needs. Notably, rates of EHR documentation were higher among physicians whose organization participates in at least one value-based care initiative—which often incorporate financial incentives for providers to screen for and address health-related social needs (5)—and among physicians serving vulnerable populations—who may have greater awareness of the social risk factors present in their community and how they impact patients’ health and care.
Structured documentation was also more common among family physicians who believe their clinic has resources available to address social needs, which indicates a relationship between how data are captured and whether this information can be used for various purposes. The use of structured methods can enable providers to more easily coordinate with and share data with other providers or community-based organizations to connect patients to social services and address immediate unmet social needs. Finally, family physicians using one of the top three EHR vendors by market share had higher rates of documentation overall and using structured methods compared to those using smaller vendors. This may be due to greater availability of standardized screening tools and templates integrated into EHRs for these larger vendors, enabling higher rates of structured data collection.
While nearly all family physicians in our study felt it was very or somewhat important to have access to external SDOH data that can help inform patient care, rated importance of having access to SDOH from outside organizations was higher among physicians serving vulnerable patient populations and among those who reported their clinic has resources to address social needs. Consistent with findings from a recent study demonstrating a positive relationship between the availability of programs or strategies at US hospitals and rates of screening and use of data on patients’ health-related social needs (6), this finding suggests perceived importance may be related to clinics’ ability to address social needs or the prevalence of unmet social needs and social risk factors in the community. Without the capacity or resources to effectively address patients’ social needs or community SDOH, physicians may place lower importance on having access to these data (7).
To help ensure that data collected and obtained are actionable and represented consistently, there are several ongoing federal and federally supported efforts to promote the standardization and exchange of structured SDOH and social needs data elements. These include standards developed by the Gravity Project to represent SDOH terminology which enable data to be captured in a standardized format in EHRs (8). Additionally, the United States Core Data for Interoperability (USCDI) includes structured SDOH data elements and specifies standards for capturing screening or assessment, problems or concerns, and goals using LOINC and SNOMED standard terminologies and ICD-10-CM Z codes, the diagnosis codes used to document SDOH (9). In 2023, the Office of the Assistant Secretary for Technology Policy/Office of the National Coordinator for Health Information Technology (ASTP) released an SDOH Information Exchange Toolkit to support stakeholders’ use of consensus-based standards by providing resources, such as a list of standardized screening tools/toolkits, and other guidance for implementing IT infrastructure that supports SDOH data exchange (10).
Continued measurement of how physicians document and obtain health equity data is important for understanding the extent to which these data can be incorporated into online medical records and clinical workflows, and can then be exchanged or utilized for various purposes including to inform further assessment or screening and contribute to shared decision-making and care delivery. Future efforts are needed to understand how often structured data elements are mapped to consensus-based standards, as this enables more consistent documentation, and facilitates the exchange of health equity data with other providers and community partners. Further, more work is needed to identify factors that influence the value of having access to external SDOH data which, combined with social needs data collected and documented internally, can help inform an individual’s care plan and facilitate the delivery of person-centered care.
DATA SOURCES AND METHODS
Data come from three waves (2022-2024) of the American Board of Family Medicine’s Continuous Certification Questionnaire, which includes family physicians who provide direct patient care. The survey was completed by 4,247 physicians in 2022 (of which 4,154 use an EHR), 8,390 physicians in 2023 (of which 8,196 use an EHR), and 7,765 physicians in the Spring recertification cohort of 2024 (of which 7,620 use an EHR). Completion of the questionnaire is required as part of ABFM’s recertification process and thus had a 100% response rate.
To mitigate burden associated with the questionnaire, certain questions were assigned to modules with approximately 50% of respondents assigned to Module A and 50% assigned to Module B. The respondent population for each year and module is included in the table below for family physicians who reported they use an EHR, which is the relevant denominator for all questions examined in this brief.
DATA AVAILABILITY
American Board of Family Medicine (ABFM) Continuous Certification Questionnaire data may be accessed for IRB-approved projects subject to the approval of the ABFM Research Governance Board. If you have questions or would like to learn more about the data source or these findings, you may contact ASTP_Data@hhs.go
REFERENCES
- American Academy of Family Physicians. Advancing Health Equity by Addressing the Social Determinants of Health in Family Medicine (Position Paper). Accessed on: July 19, 2024. Available from: https://www.aafp.org/about/policies/all/social-determinants-health-family-medicine-position-paper.html.
- Grumbach K, Hart LG, Mertz E, Coffman J, Palazzo L. Who is caring for the underserved? A comparison of primary care physicians and nonphysician clinicians in California and Washington. Ann Fam Med. 2003 Jul-Aug;1(2):97-104. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1466573/
- The Office of the Assistant Secretary for Technology Policy. Advancing Health Equity Fact Sheet. 2024 [Accessed on: July 19, 2024]. Available from: https://www.healthit.gov/sites/default/files/2024-03/Health_Equity_Fact_Sheet.pdf.
- Iott BE, Patel V, Richwine C. Physician Documentation of Social Determinants of Health: Results from Two National Surveys. J Gen Intern Med (2024). Available from: https://link.springer.com/article/10.1007/s11606-024-09184-w
- Health Care Transformation Task Force. Value-based Payment Models: A Catalyst for Addressing the Non-Medical Factors that Influence Health. January 2018. Accessed on: Accessed July 19, 2024. Available from: https://hcttf.org/value-and-sdoh/
- Richwine C, Meklir S. Hospitals' collection and use of data to address social needs and social determinants of health. Health Serv Res. 2024 Jul 2. Available from: https://pubmed.ncbi.nlm.nih.gov/38952231/
- DesRoches CM, Wachenheim D, Garcia A, et al. Clinician and Patient Perspectives on the Exchange of Sensitive Social Determinants of Health Information. JAMA Netw Open. 2024;7(10):e2444376. Available from: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2825509?resultClick=1
- Health Level 7. Gravity Project. Accessed on: July 26, 2024. Available from: https://www.hl7.org/gravity/
- Office of the Assistant Secretary for Technology Policy. United States Core Data for Interoperability (USCDI): Social Determinants of Health [Internet]. Accessed on: July 26, 2024. Available from: https://www.healthit.gov/isa/uscdi-data-class/social-determinants-health.
- Office of the Assistant Secretary for Technology Policy. Social Determinants of Health Information Exchange Toolkit: Foundational Elements for Communities. February 2023 [Accessed on: July 26, 2024]. Available from: https://www.healthit.gov/sites/default/files/2023-02/Social%20Determinants%20of%20Health%20Information%20Exchange%20Toolkit%202023_508.pdf.
ACKNOWLEDGMENTS
The authors are with the Office of Standards, Certification, and Analysis, within the Office of the Assistant Secretary for Technology Policy (ASTP). The data brief was drafted under the direction of Mera Choi, Director of the Technical Strategy and Analysis Division, Vaishali Patel, Deputy Director of the Technical Strategy and Analysis Division, and Wesley Barker, Chief of the Data Analysis Branch with subject matter expertise from Samantha Meklir and JaWanna Henry.
SUGGESTED CITATION
Richwine C. Family Medicine Physicians' Documentation Methods and the Value of Access to External Data for Addressing Social Needs. Office of the Assistant Secretary for Technology Policy. Data Brief: 76. 2024.
APPENDIX
Appendix Table 1: Survey questions used for analyses and respondent population.
Survey Question | Response Options | Respondent Population |
|---|---|---|
Rate your sense of the general importance of accessing the following types of external patient information electronically (within your EHR and/or portal): Access to social determinants of health information (e.g., housing stability, food insecurity) from other health systems/organizations) | Very important Somewhat important Not at all important | 2022-2023: Module A only (50%) 2024: Not asked Note: Not asked to respondent who indicated they do not use an EHR |
How often do you document screening for social needs (such as transportation, housing, food insecurity) in your primary outpatient EHR… by checking a box/button within the EHR? by writing it in a note? By entering it as a diagnosis (i.e., ICD-10-CM Z codes)? | Often Sometimes Rarely Never Don’t know | 2022-2023: Module B only (50%) 2024: All respondents Note: Not asked to respondent who indicated they do not use an EHR |
My clinic has the resources and tools, such as dedicated staff and linkages to community programs, to address patients' social needs | Agree Neutral Disagree | 2022-2024: All respondents |
Source: 2022-2024 American Board of Family Medicine Continuous Certification Questionnaire
Appendix Table 2: Combination of methods family physicians often or sometimes use to document screening for social needs in primary outpatient EHR, 2022-2024 (pooed).
Methods of documentation | |
|---|---|
Single method: | |
Free-text notes | 16% |
Checkbox/button | 9% |
Diagnosis codes | 1% |
Multiple methods: | |
Free-text notes and Checkbox/button | 13% |
Free-text notes and Diagnosis codes | 9% |
Checkbox/button and Diagnosis codes | 3% |
Free-text notes, Checkbox/button, and Diagnosis codes | 22% |
Do not document in EHR | 27% |
Total | 100% |
Source: 2022-2024 American Board of Family Medicine Continuous Certification Questionnaire
Notes: The denominator represents a pooled sample of family physicians from 2022-2024 who use an EHR (N = 13,795). This includes Module B respondents in 2022-2023 (N = 6,175) and all respondents in 2024 (N = 7,620).
Appendix Figure 1: Family physicians’ beliefs that their clinic has resources available to address patients' social needs, 2022-2024
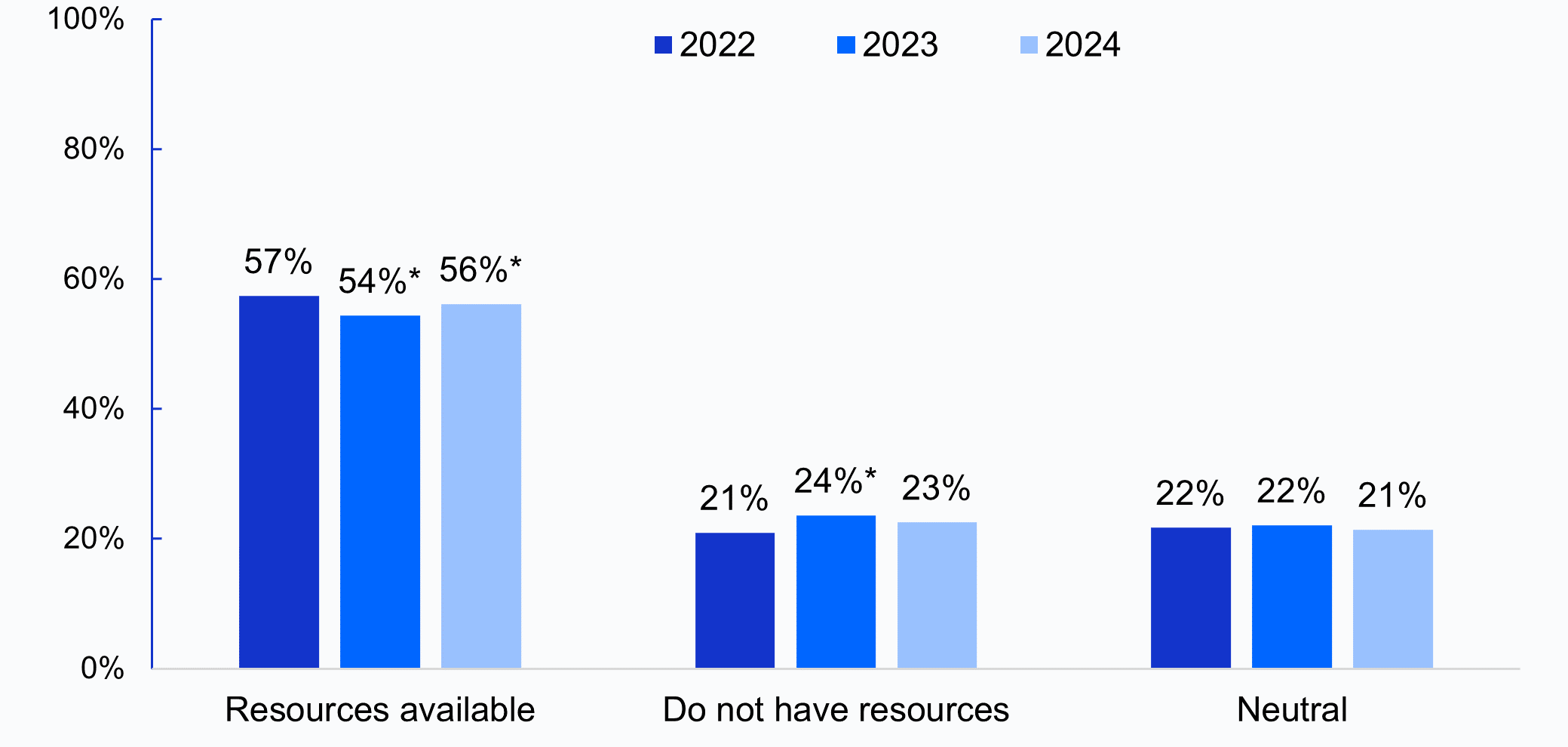
Source: 2022-2024 American Board of Family Medicine Continuous Certification Questionnaire
Notes: Denominator represents all respondents in 2022-2024. Respondents were asked to indicate their level of agreement with the statement, “My clinic has the resources and tools, such as dedicated staff and linkages to community programs, to address patients' social needs”: Resources available = “Agree”, Do not have resources = “Disagree”, Neutral = “Neutral” (neither agree nor disagree). *Indicates statistically significant difference from prior year (P<.05).