Electronic prescribing of controlled substances (EPCS) enables clinicians to securely transmit prescriptions for controlled substances to a pharmacy (1). Prescription drug monitoring programs (PDMPs) are electronic databases that contain patient-specific prescription information, which enables clinicians to view their patients’ prescription history before prescribing contolled substances (2). Together, the use of EPCS and PDMPs can help clinicians make informed treatment decisions. However, these tools are only useful if EPCS is used routintely, and if clinicians check the PDMP prior to prescribing. Recent efforts, such as federally mandated use of EPCS technology (3) and integration of PDMPs into electronic health record (EHR) sytems, have aimed to increase the utility of information contained in PDMPs. This brief provides national estimates of office-based physicians’ use of EPCS and PDMPs in 2021 and explores variation in use by physician characteristics—including specialty, practice size, and frequency of prescribing controlled substances—and describes physician-reported benefits associated with PDMP use.
HIGHLIGHTS
- The share of office-based physicians who reported using EPCS “often” increased significantly between 2019 and 2021, from 37% to 62%. However, EPCS use varied by specialty, practice size, ownership, and EHR developer market share.
- PDMP use remained relatively stable between 2019 and 2021, with 65% of physicians reporting they checked the PDMP “often” prior to prescribing controlled substances to a patient for the first time in 2021.
- Hospitals that experienced major public health reporting challenges in 2019 were less likely to be engaged in certain types of electronic public health reporting in 2021.
- The share of physician prescribers who accessed the PDMP through their EHR (rather than a portal or secure website) increased by 62% between 2019 and 2021.
- Most physicians who checked their state’s PDMP reported experiencing at least 1 benefit associated with use.
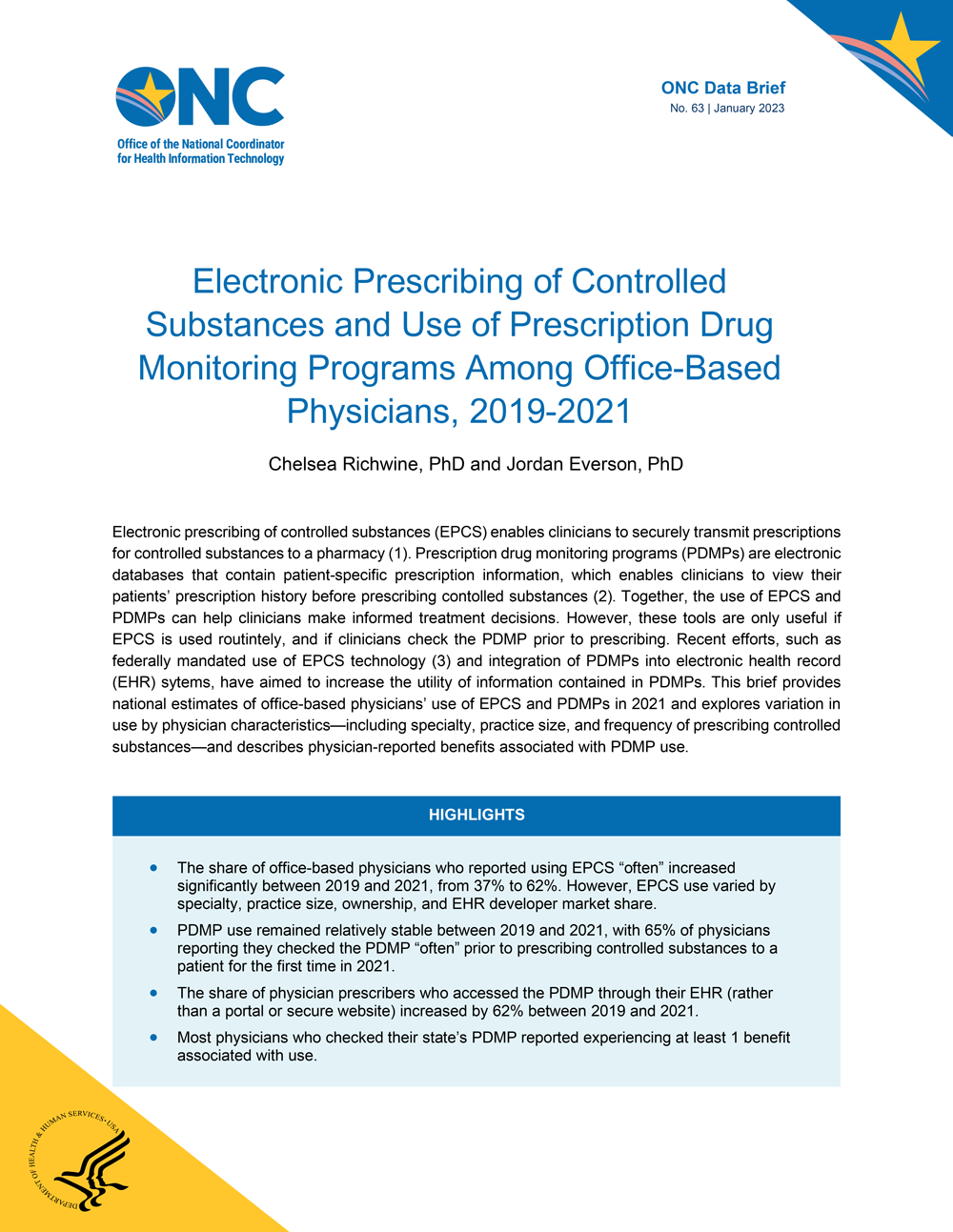
In 2021, the share of physicians who used EPCS “often” when prescribing controlled substances nearly doubled from 37% to 62%.
FINDINGS
★ Seventy-one percent of office-based physicians who prescribe controlled substances reported using EPCS “often” or “sometimes” in 2021 with 62 percent reporting they use EPCS “often” – a significant increase from just over one-third of physician prescribers in 2019 (37%).
★ In 2021, more than three-quarters (78%) of office-based physicians who prescribe controlled substances reported checking their state’s PDMP “often” or “sometimes” prior to prescribing controlled substances, with 65 percent reporting they check the PDMP “often” – a slight increase from 62 percent of physician prescribers in 2019.
★ The share of physician prescribers who “rarely” or “never” use EPCS declined significantly over the last 2 years, from 55 percent in 2019 to 26 percent in 2021.
Figure 1: Physician-reported frequency of checking the PDMP and using EPCS (among those who prescribe controlled substances), 2019-2021
Source: 2019-2021 National Electronic Health Records Survey.
Notes: Denominator represents office-based physicians who prescribe controlled substances (N=1,393, 91% in 2019 and N=1,705, 90% in 2021). Respondents who indicated they “don’t know” whether they check their PDMP (5% in 2019, 6% in 2021) or use EPCS (1% in 2019, 2% in 2021) were excluded. See the Definitions page for descriptions of key terms and Appendix Table A1 for underlying survey questions. *Indicates statistically significant difference between 2019 and 2021 (p<0.05).
More frequent prescribers of controlled substances were more likely to use EPCS technology compared to those who prescribe less frequently.
FINDINGS
★ In 2021, nearly two-thirds of physicians reported they “often” or “sometimes” prescribed controlled substances (28% and 37%, respectively). About a quarter “rarely” prescribed controlled substances (24%)—a significant decrease from 2019 (Appendix Table A2)—and only 10 percent “never” prescribed.
★ Physicians who “often” presribed controlled substances checked the PDMP (85%) and used EPCS at higher rates (88%) compared to those who “sometimes” (79% for both PDMP and EPCS) or “rarely” (69% PDMP, 41% EPCS) prescribed controlled substances.
★ Despite similar rates of prescribing in the last 3 years, the share of physicians using EPCS increased significantly between 2019 and 2021 for both frequent and infrequent prescribers of controlled substances (Appendix Table A3); whereas the share of physicians who check the PDMP only increased among those who rarely prescribe (Appendix Table A4).

Figure 2: Percent of office-based physicians that check the PDMP (Panel A) and use EPCS technology (Panel B), by frequency of prescribing controlled substances, 2021.
Source: 2021 National Electronic Health Records Survey.
Notes: The inner ring in both panels represents physician-reported frequency of prescribing controlled substances (often / sometimes / rarely / never). The outer ring of the left panel represents the share of office-based physicians who often or sometimes check the PDMP vs. rarely or never check the PDMP (“No PDMP”) within each level of prescribing. The outer ring of the right panel represents the share of office-based physicians who often or sometimes use EPCS vs. rarely or never use EPCS (“No EPCS”) within each level of prescribing.
Physicians’ use of EPCS varied significantly by practice characteristics.
FINDINGS
★ Rates of PDMP use were higher among primary care physicians (compared to surgical specialists) and among physicians working in hospital-owned (relative to physician-owned) practices. Underlying data tables are available in Appendix Table A5.
★ Rates of EPCS use were higher among primary care physicians (compared to medical and surgical specialists) and among physicians with a large market share EHR developer.
★ Rates of EPCS use were lower among solo practitioners compared to practices with 4 or more physicians.
★ Rates of EPCS were also lower among physician-owned practices compared to other ownership types.
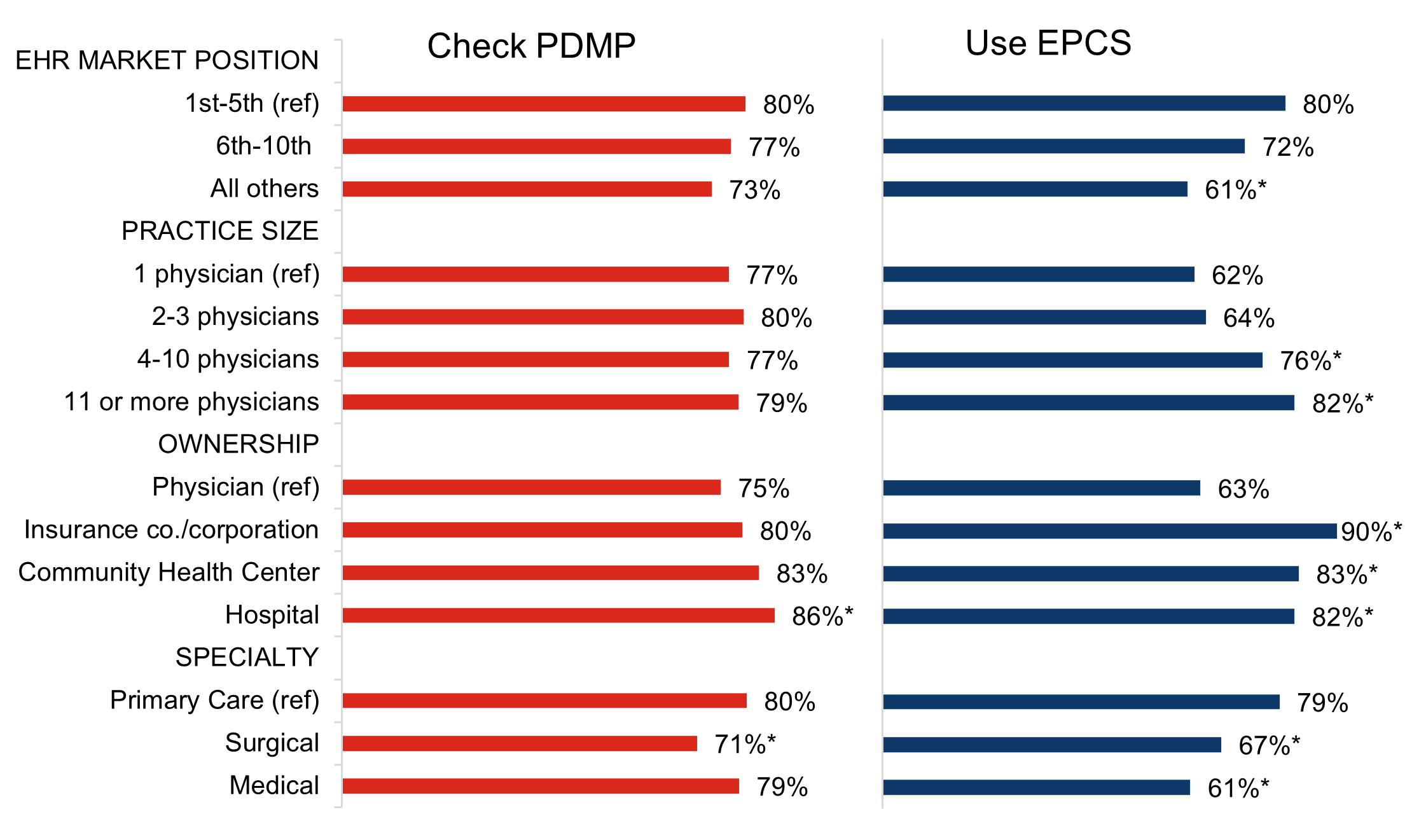
Figure 3: Percent of office-based physician who check the PDMP and use EPCS (among those who prescribe controlled substances), by practice characteristics, 2021.
Source: 2021 National Electronic Health Records Survey.
Notes: Use EPCS is defined as "often" or "sometimes" using EPCS. Check the PDMP is defined as "often" or "sometimes" checking the PDMP before prescribing controlled substances. See the Definitions page for descriptions of key terms. Missing responses (N=4) and "other" ownership types (N=64) were excluded from the denominator. EHR market position refers to EHR developer market share. Missing (N=5), “don’t know” (N=6), and N/A (i.e., do not use EHR) (N=156) responses were excluded from the denominator. * Indicates statistically significant from reference group (p<0.05).
The share of physician prescribers of controlled substances who accessed the PDMP through their EHR increased significantly between 2019 and 2021.
FINDINGS
★ In 2021, more than one-third of physician prescribers of controlled substances accessed their PDMP through their EHR (34%) – a 62 percent increase from 2019 (21%).
★ In both years, most prescribers reported accessing the PDMP using a system outside of an EHR, such as a PDMP portal or secure website (Appendix Table A6).
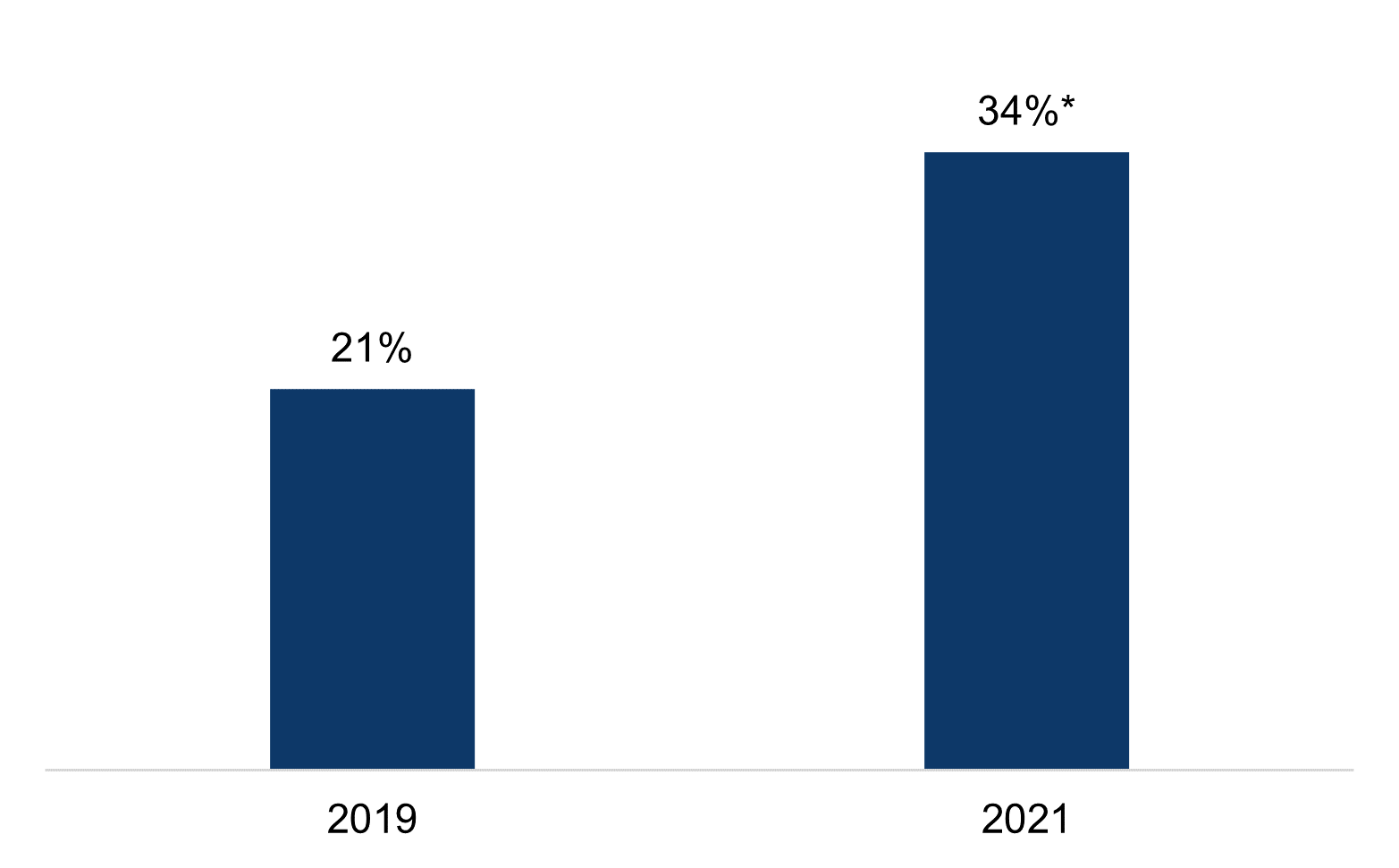
Figure 4: Percent of office-based physicians who accessed the PDMP through their EHR (among those who prescribe controlled substances and check their state's PDMP), 2019-2021.
Source: 2019-2021 National Electronic Health Records Survey.
Notes: Denominator represents office-based physicians who prescribe controlled substances and check their state's PDMP.
The share of physicians who accessed the PDMP via their EHR varied widely by EHR developer.
FINDINGS
★ In 2021, the share of physicians who accessed the PDMP via their EHR varied by EHR developer, ranging from four percent of Practice Fusion users to 56 percent of Epic users.
★ Physicians with an EHR developed by Epic, athenahealth, NextGen, e-MDs, Cerner, or eClinicalWorks accessed the PDMP through their EHR at higher rates (ranging from 35% to 56%) than the national average (34%).
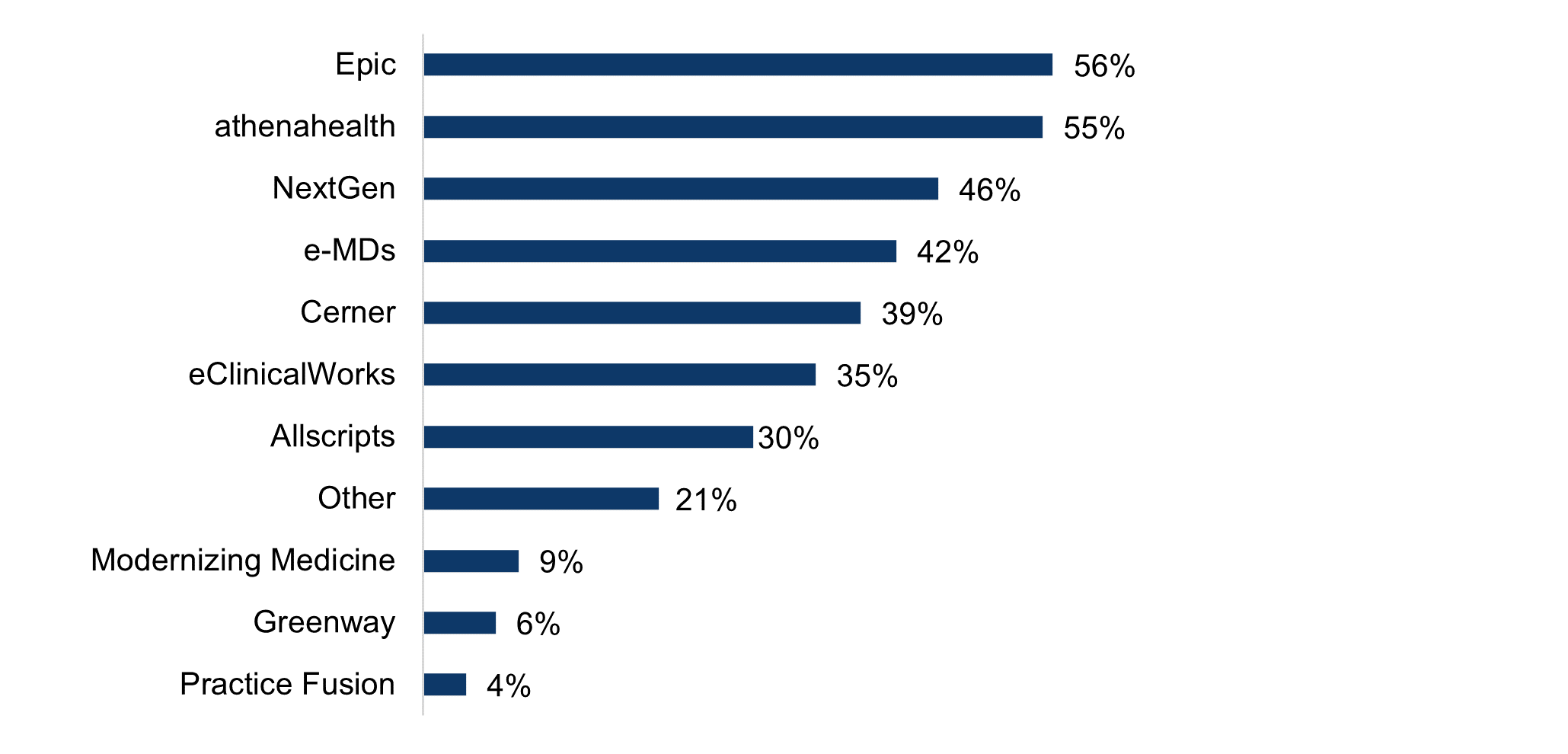
Figure 5: Percent of office-based physicians who access the PDMP through their EHR (among those who prescribe controlled substances and check their state's PDMP), by EHR vendor, 2021.
Source: 2021 National Electronic Health Records Survey.
Notes: Denominator represents office-based physicians who prescribe controlled substances and check their state's PDMP. Missing (N=4), "don't know" (N=3), and not applicable (i.e., do not use an EHR, N=125) responses were excluded.
In 2021, about 3 in 10 physician prescribers and PDMP users indicated they typically request to view PDMP data from other states prior to prescribing controlled substances.
FINDINGS
★ In 2021, only 29 percent of physicians who prescribe controlled substances and check their state’s PDMP indiciated they typically request to view PDMP from other states prior to prescribing a controlled substance to a patient for the first time, whereas 20 percent indiciated they “don’t know” whether this request was typically made.
★ The share of physicians who typically request to view PDMP data from other states prior to prescribing did not change significantly between 2019 and 2021.
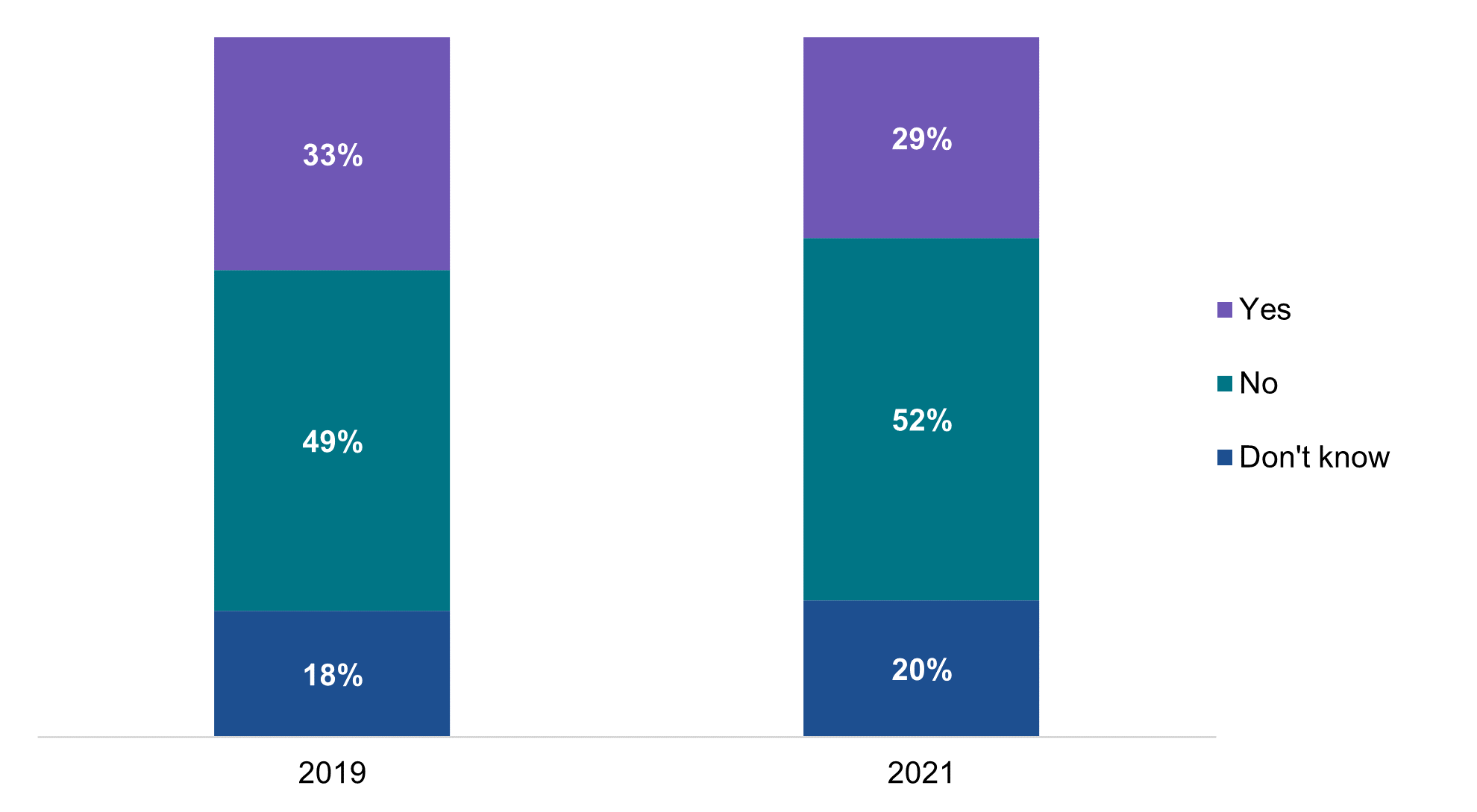
Figure 6: Percent of office-based physicians who typically request to view PDMP data from other states prior to prescribing a controlled substance to a patient for the first time (among those who prescribe controlled substances and check their state's PDMP), 2019-2021.
Source: 2019-2021 National Electronic Health Records Survey.
Notes: Denominator represents office-based physicians who prescribe controlled substances and check their state's PDMP. Missing responses were excluded from the denominator (N = 37).
Most physicians who checked their state’s PDMP reported experiencing at least 1 benefit associated with use.
FINDINGS
★ More than half of physician prescribers of controlled substances who checked their state’s PDMP reported they “reduced or eliminated controlled substance prescriptions for a patient” (59%) or “confirmed appropriateness of treatment” (54%) as a result of PDMP use.
★ Other commonly reported benefits associated with PDMP use included “confirming patients’ misuse of prescriptions” (43%) and “changing controlled substance prescriptions to non-opioid pharmacologic” (36%); whereas prescribing naloxone and assessing pain and function of a patient (e.g., PEG) were less common (13% and 18%, respectively).
★ On average, physician prescribers and PDMP users reported about 3 distinct benefits associated with PDMP use in 2021.
| PDMP Benefits | |
|---|---|
| Reduced or eliminated controlled substance prescriptions for a patient | 59% |
| Confirmed appropriateness of treatment | 54% |
| Confirmed patients’ misuse of prescriptions (e.g., engage in doctor shopping) | 43% |
| Changed controlled substance prescriptions to non-opioid pharmacologic (e.g., NSAIDS or acetaminophen) or non-pharmacologic therapy (e.g., exercise/physical therapy or CBT). | 36% |
| Consulted and/or coordinate with other members of the care team | 26% |
| Referred additional treatment (e.g., substance abuse treatment, psychiatric or pain management) | 28% |
| Consulted with other prescribers listed in PDMP report | 23% |
| Assessed pain and function of patient (e.g., PEG) | 18% |
| Prescribed naloxone | 13% |
| At least 1 reported benefit | 87% |
| Mean number of benefits | 3.0 |
Table 1: Physician-reported benefits associated with PDMP use (among those who prescribe controlled substances and check their state's PDMP), 2021
Source: 2021 National Electronic Health Records Survey.
Notes: Denominator represents office-based physicians who prescribe controlled substances and check their state's PDMP.
Summary
In 2021, more than two-thirds of physicians who prescribed controlled substances used EPCS technology (71%) and more than three-quarters checked their state’s PDMP (78%) prior to prescribing controlled substances to a patient for the first time. While PDMP use remained relatively stable from 2019 to 2021, the percentage of prescribers who reported using EPCS “often” increased significantly from 37% to 62%. The share of prescribers who reported rarely or never using EPCS decreased significantly from 55% to 26%. Further, physicians who more often prescribed controlled substances were more likely to use EPCS. Given the stringent requirements for setting up EPCS (4), infrequent prescribers may have had less motivation to implement such technology unless it was mandated in their state (5). Almost 90% of physicians that used the PDMP reported experiencing a benefit from its use, and on average physicians reported experiencing three distinct benefits. Taken together, these data indicate that EPCS and PDMP use were both widespread and provided substantial benefit.
Despite the significant progress in the use of EPCS among office-based physicians, rates of EPCS use varied significantly by physician specialty, practice size, ownership, and EHR developer market share.
For instance, 2021 rates of EPCS use among physicians working in community health centers more than tripled from 2017 rates (6) and were significantly higher than among physicians working in physician-owned practices. These high rates of engagement may be attributable to funding community health centers received from the Health Resources & Services Administration (HRSA) to support the adoption and advancement of health IT (7) or other similar funding opportunities. This suggests that targeted support may be needed to achieve universal use among physicians in lower-resource settings. PDMP use was less correlated with practice characteristics, potentially because it is not as dependent on support of EHR developers or the resources the practice can commit to implementation.
The integration of PDMPs within EHRs is one effort to promote data sharing and use for authorized users, and may help physician prescribers of controlled substances realize broader benefits from PDMP use as prior work has shown more frequent PDMP use among physicians whose PDMP is integrated with their EHR (8). Yet in contrast to the high level of use of the PDMP and EPCS, the share of physicians who accessed the PDMP through their EHR was relatively low but had increased substantially from 2019. These data indicate the effectiveness of efforts to increase integration and the importance of continuing those efforts (9). Substantial variation by EHR developer indicates that progress is likely not occurring evenly, and that limited capacity of some EHR developers and PDMP developers to support the integration of PDMPs into EHR systems is likely a barrier to its uptake.
Finally, despite physicians’ widespread access to data from their state’s PDMP, the electronic sharing of PDMP data across state lines remains limited and did not change between 2019 and 2021. Querying other state PDMPs – especially bordering states – can be important to capture complete prescription histories of patients who have sought care in different health care systems and geographic locations (10). Interstate querying is one of the major remaining hurdles for PDMP interoperability. As of 2021, most PDMPs were connected to an interstate hub for PDMP data exchange, but only 28 states/territories reported sharing data with more than 30 other states (11). It is worth noting that the share of physicians who check the PDMP and view PDMP data from other states may be shaped by several dynamics at the state or local level: local differences in the perceived value of checking other states (e.g., because of proximity to borders), prescriber use laws that describe the circumstances under which health care providers are required to check the PDMP (12), the capabilities of the PDMP to query neighboring and other states , and the active adoption and use of interstate hubs for PDMP data exchange or the ability to access PDMP data by other means (e.g., through Health Information Exchange organizations).
DEFINITIONS
Electronic Prescribing of Controlled Substances (EPCS) – technology that enables prescribers to securely transmit prescriptions for controlled substances to a pharmacy (1).
EPCS use – physicians’ use of EPCS is defined as sending prescriptions for controlled substances electronically to the pharmacy.
Hospital ownership – includes practices owned by medical/academic health centers and other hospital types.
Insurance company or corporation ownership – includes practices owned by insurance companies, health plans, or HMOs and other health care corporations.
Prescription Drug Monitoring Program (PDMP) – electronic databases that contain patient-specific prescription information, which enables clinicians to view their patients’ prescription dispense history before prescribing contolled substances (2).
PDMP use – physician (or designated staff) use of the PDMP is defined as checking the PDMP prior to prescribing controlled substances to a patient for the first time.
Data Source and Methods
Data come from the 2019 and 2021 National Electronic Health Records Survey (NEHRS). The NEHRS is an annual survey of office-based physicians conducted by the Centers for Disease Control and Prevention’s National Center for Health Statistics. Physicians included in this survey provide direct patient care in office-based practices and community health centers; excluded are those who do not provide direct patient care (radiologists, anesthesiologists, and pathologists).
Among the 10,302 physicians that were initially recruited to complete the 2019 and 2021 surveys, 5,684 were deemed ineligible in 2019 and 3,177 were deemed ineligible in 2021. Among those who were eligible or whose eligibility could not be determined, NCHS estimated an unweighted response rate of 41 percent in 2019 and 47 percent in 2021, yielding a final sample of 1,524 respondents in 2019 and 1,875 respondents in 2021.
Adjustments were made to account for non-response among physicians whose eligibility could not be determined and for those who did not participate in the survey. Responses for the 1,524 records included in the final 2019 survey were weighted to reflect national estimates for approximately 301,603 office-based physicians in the U.S. Responses for the 1,875 records included in the final 2021 survey were weighted to reflect national estimates for approximately 403,013 office-based physicians in the U.S.
Additional survey documentation can be found on the NEHRS website.
References
- Office of the National Coordinator for Health IT. Health IT Playbook. Section 4. Opioid Epidemic & Health IT. https://www.healthit.gov/playbook/opioid-epidemic-and-health-it/
- Centers for Disease Control and Prevention. Prescription Drug Monitoring Programs (PDMPs): What States Need to Know. https://www.cdc.gov/drugoverdose/pdmp/index.html
- Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment (SUPPORT) for Patients and Communities Act, Section 2003. https://www.congress.gov/bill/115th-congress/house-bill/6/text
- Drug Enforcement Agency. Interim Final Rule. Electronic Prescribing of Controlled Substances. https://www.deadiversion.usdoj.gov/fed_regs/rules/2010/fr0331.htm
- State Mandates Driving EPCS and PDMP Utilization. Accessed October 6, 2022. https://drfirst.com/resources/regulatory-mandates/
- Johnson C. & Estrada M. (June 2022). Electronic Prescribing of Controlled Substances Among Office-Based Physicians, 2017-2019. ONC Data Brief, no.58. Office of the National Coordinator for Health Information Technology: Washington DC.
- Zur J., Tolbert J., Sharac J., & Markus A. (July 2018). The Role of Community Health Centers in Addressing the Opioid Epidemic. Kaiser Family Foundation Issue Brief. https://files.kff.org/attachment/Issue-Brief-The-Role-of-Community-Health-Centers-in-Addressing-the-Opioid-Epidemic.
- Richwine, C., & Everson, J. (2022). National Estimates and Physician-Reported Impacts of Prescription Drug Monitoring Program Use. Journal of General Internal Medicine, 1-8.Integration Taxonomy: Advancing PDMP-EHR Integration Project PDMP-EHR Integration Toolkit. https://www.healthit.gov/sites/default/files/page/2022-08/Integration_Taxonomy.pdf
- Prescription Drug Monitoring Program Training and Technical Assistance Center. (January 2021). Interstate PDMP Access and Data Sharing Alignment. https://www.pdmpassist.org/pdf/resources/Interstate_PDMP_Access_and_Data_Sharing_Alignment_20210125.pdf
- The Pew Charitable Trusts. (January 2018). When Are Prescribers Required to Use Prescription Drug Monitoring Programs? https://www.pewtrusts.org/en/research-and-analysis/data-visualizations/2018/when-are-prescribers-required-to-use-prescription-drug-monitoring-programs
- Prescription Drug Monitoring Program Training and Technical Assistance Center (2021). PDMP Policies and Capabilities. Accessed January 2023. https://www.pdmpassist.org/Policies/Maps/PDMPPolicies
- Prescription Drug Monitoring Program Training and Technical Assistance Center. (July 2020). Mandatory Enrollment and Use of PDMPs. https://www.pdmpassist.org/pdf/TAG_Mandatory_Enrollment_Use_20200710.pdf
Acknowledgements
The authors are with the Office of Technology, within the Office of the National Coordinator for Health Information Technology. Lolita Kachay and Carmen Smiley, also with the ONC Office of Technology, contributed to the brief. The data brief was drafted under the direction of Mera Choi, Director of the Technical Strategy and Analysis Division, Vaishali Patel, Deputy Director of the Technical Strategy and Analysis Division, and Wesley Barker, Chief of the Data Analysis Branch.
Suggested Citation
Richwine C. & Everson J. (January 2023). Title. ONC Data Brief, no.63. Office of the National Coordinator for Health Information Technology: Washington DC.
Appendix
Appendix Table A1: Survey questions assessing physicians’ frequency of prescribing controlled substance, using EPCS, and accessing their state’s PDMP
|
Measure |
Question Text |
Response Options |
|---|---|---|
|
Prescribe controlled substances |
How frequently do you prescribe controlled substances? |
|
|
Use electronic prescribing of controlled substances (EPCS) |
How frequently are prescriptions for controlled substances sent electronically to the pharmacy? |
|
|
Check prescription drug monitoring program (PDMP) |
How frequently do you or designated staff check your state’s prescription drug monitoring program (PDMP) prior to prescribing a controlled substance to a patient for the first time? |
|
|
PDMP access method |
How do you or your designated staff check your state’s PDMP? |
|
|
Interstate data sharing |
When checking your state’s PDMP, do you or designated staff typically request to view PDMP data from other states prior to prescribing a controlled substance for the first time? |
|
Source: 2019-2021 National Electronic Health Records Survey.
Notes: For the EPCS measure, the “rarely” and “never” response options were combined in the 2019 survey.
Appendix Table A2: Physician-reported frequency of prescribing controlled substances, 2019-2021.
| 2019 | 2021 | |
|---|---|---|
| Often | 29% | 28% |
| Sometimes | 31% | 37%* |
| Rarely | 31% | 24%* |
| Never | 8% | 10% |
| Blank | 0% | 0% |
| Don’t know | 1% | 0% |
Source: 2019-2021 AHA Annual Survey Information Technology Supplement.
Note: *Statistically significant from 2019 (p<0.05).
Appendix Table A3: Percent of office-based physicians that use EPCS, by frequency of prescribing controlled substances, 2019-2021.
| 2019 | 2021 | |
|---|---|---|
| Often | 60%* | 88%* |
| Sometimes(reference) | 49% | 79% |
| Rarely | 24%* | 41%* |
Source: 2019-2021 AHA Annual Survey Information Technology Supplement.
Note: Only includes those who prescribe controlled substances. *Statistically significant from “Sometimes” reference group (p<0.05). Bold text indicates statistically significant from 2019 (p<0.05).
Appendix Table A4: Percent of office-based physicians that check the PDMP, by frequency of prescribing controlled substances, 2019-2021.
| 2019 | 2021 | |
|---|---|---|
| Often | 85% | 85% |
| Sometimes (reference) | 82% | 79% |
| Rarely | 59%* | 69%* |
Source: 2019-2021 AHA Annual Survey Information Technology Supplement.
Note: Only includes those who prescribe controlled substances. *Statistically significant from “Sometimes” reference group (p<0.05). Bold text indicates statistically significant from 2019 (p<0.05).
Appendix Table A5: Percent of office-based physician prescribers of controlled substances that use EPCS technology and check their PDMP, by practice characteristics, 2021.
| Practice characteristics | Use EPCS | Check PDMP |
|---|---|---|
| Practice size | ||
| 1 physician (reference) | 62% | 77% |
| 2-3 physicians | 64% | 80% |
| 4-10 physicians | 76%* | 77% |
| 11 or more physicians | 82%* | 79% |
| Practice ownership | ||
| Physician/Physician group (reference) | 63% | 75% |
| Insurance company or corporation | 90%* | 80% |
| Community Health Center | 83%* | 83% |
| Hospital | 82%* | 86%* |
| Specialty | ||
| Primary Care (reference) | 79% | 80% |
| Surgical | 67%* | 71%* |
| Medical | 61%* | 79% |
| Setting | ||
| Private solo or group practice (reference) | 67% | 77% |
| Other setting | 82%* | 80% |
| Medicare Physicians | ||
| Treat Medicare Patients | 71% | 79% |
| Do Not Treat Medicare Patients | 72% | 71%* |
| Medicaid Physicians | ||
| Treat Medicaid Patients | 73% | 78% |
| Do Not Treat Medicaid Patients | 67% | 79% |
| EHR Vendor Market Share | ||
| 1st-5th market position (reference) | 80% | 80% |
| 6th-10th market position | 72% | 77% |
| All others | 61%* | 73% |
Source: 2021 AHA Annual Survey Information Technology Supplement.
Note: Use EPCS is defined as "often" or "sometimes" using EPCS technology. Check the PDMP is defined as "often" or "sometimes" checking the PDMP before prescribing controlled substances. "Insurance company or corporation" ownership includes insurance companies, health plans, or HMOs and other health care corporations. "Hospital" ownership includes medical/academic health centers and other hospital types. Missing responses (N=4) and "other" ownership types (N=64) were excluded from the denominator. For Medicare and Medicaid physicians, “don’t know” (N=13 and 12, respectively) and missing (N=8 and 3, respectively) responses were coded as “Do not treat”. For EHR developer market share, missing (N=5), “don’t know” (N=6), and N/A (i.e., do not use EHR) (N=156) responses were excluded from the denominator. * Indicates statistically significant from reference group (p<0.05).
Appendix Table A6: Physician-reported frequency of sending prescriptions for controlled substances electronically to the pharmacy, 2019-2021.
| 2019 | 2021 | |
|---|---|---|
| Use EHR system | 21% | 34%* |
| Use system outside of EHR | 71% | 60% |
| Don’t know | 8% | 6% |
Source: 2012-2021 AHA Annual Survey Information Technology Supplement.
Note: Only includes those who prescribe controlled substances and check their state's PDMP. Use of system outside of an EHR may include a PDMP portal or secure website. *Statistically significantly different from prior year (p < 0.05).